Introduction – The Puzzle of Depression
Depression is a perplexing paradox. On the one hand, it is one of the most debilitating conditions in human experience—characterized by crushing sadness, loss of interest and energy, withdrawal from others, and sometimes suicidal thinking. On the other hand, it is astonishingly common and ancient. Globally, hundreds of millions of people (roughly 5–6% of adults) suffer from depression at any given time. If depression were purely a malfunction of the mind—a disease with no redeeming features—it is hard to explain why evolution has not eliminated such a seemingly self-defeating trait. Natural selection tends to weed out traits that are only harmful. Pain, for example, is unpleasant yet protects us from further injury; fever feels awful but helps fight infection. Could it be that, in the lives of our distant ancestors, depressive behavior sometimes served a purpose and was therefore favored by natural selection, perhaps as a social adaptation to be expressed under specific yet commonly recurring circumstances? This question lies at the heart of the Social Navigation Hypothesis (SNH) of depression.
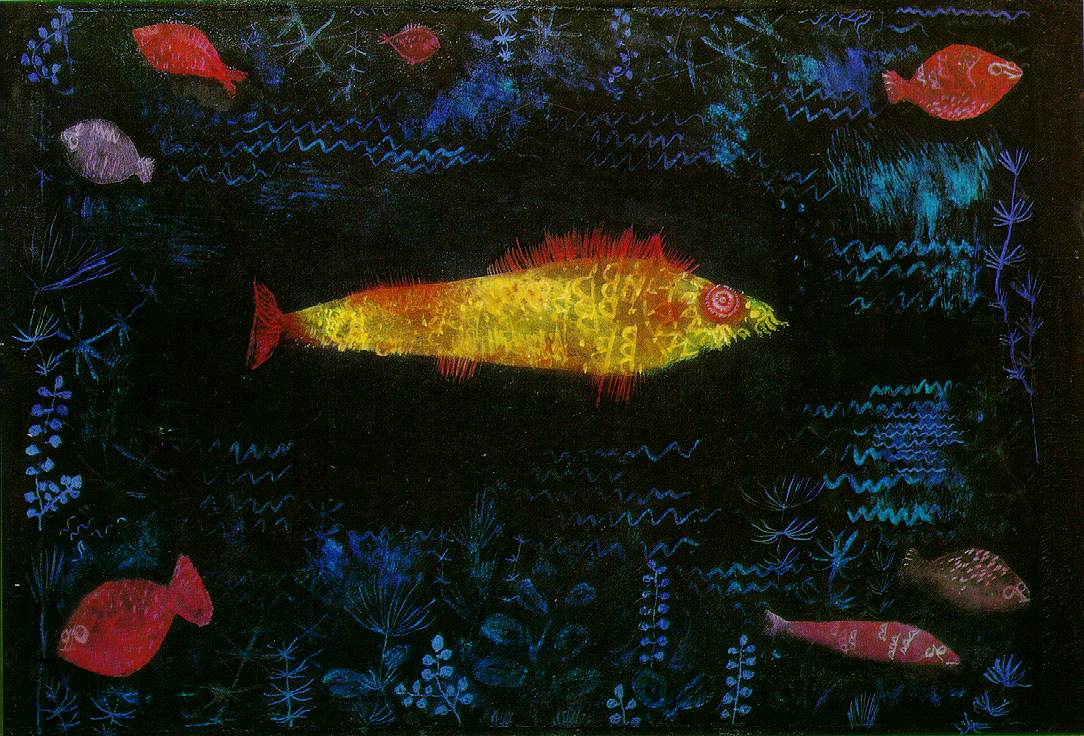
To illustrate the puzzle, imagine an elderly man who has a wealth of knowledge, resources, and love to offer his family, yet finds himself sidelined and ignored. He longs to contribute to his kin—something that would enhance his family’s and lineage’s success and give him a sense of legacy. From an evolutionary standpoint, helping one’s kin boosts what biologists call inclusive fitness (the success of relatives who share your genes—specific allelic variants—by virtue of recent common descent). But if his family refuses to value his contributions, the man is stuck in a tragic bind. Feeling useless and isolated, he becomes deeply depressed. Traditionally, we might call this a pathological reaction to loss and loneliness. An alternative view is that the depression itself—the despair, the fatigue, the withdrawal, even frightening thoughts—might function as a drastic social signal that something in the relationship has gone very wrong. In effect, the man’s collapse broadcasts an urgent message to the family: their current social arrangement is unsustainable and needs to change. His pain is palpable, his withdrawal imposes a cost on the family (they lose his usual support and must worry about him), and these outcomes might pressure them to re-engage and include him before it is too late. In this view, depression could be not just an internal illness but a form of communication—an unconscious strategy aimed at prompting a change in others’ behavior.
This provocative idea forms the basis of the Social Navigation Hypothesis. The SNH proposes that depression is not merely a brain malfunction or “mental illness,” but in part an evolved strategy for navigating complex social challenges. According to this hypothesis, depressive symptoms—including the more severe forms often called major depression—can serve highly organized adaptive functions that helped our ancestors resolve high-stakes social dilemmas. Specifically, depression may: (1) relentlessly focus the sufferer’s mind on a serious problem that demands resolution; (2) credibly signal to others that the person needs help confronting an extraordinarily complex social problem that makes the current life situation untenable; and (3) when persuasion and honest pleas for help fail, escalate to compel a useful response. In essence, depression is envisioned as a painfully hard-handed way of pressing “pause” on business-as-usual when one’s life trajectory is not working and cannot be fixed alone.
Importantly, the Social Navigation Hypothesis does not apply to every instance of low mood or sadness; it targets a distinct subset of predicaments that can be called nonpointsource social entrapment—diffuse, multiactor constraints that stubbornly block an adaptive life change, often a comprehensive socioeconomic niche change 1, unless others cooperate. These constraints are typically relational, institutional, or moral and interlock to create an unusually complex mesh of obligations and dependencies that cannot be unilaterally revised without serious social costs. The hypothesis is meant to explain depressive episodes precipitated by such persistent, distributed barriers rather than transient discouragement or simple grief over a oneoff loss. Other highstakes, cognitively demanding problems can certainly elicit low mood and analytical rumination; however, the full highgain bargaining/sanction profile proposed by SNH is expected chiefly when two conditions cooccur: (i) a credibly better alternative arrangement exists with substantial longterm inclusivefitness upside, and (ii) access to that arrangement is blocked by multiple partners who must be bargained with more or less simultaneously—essentially a herdingcats problem—requiring a high (nearly complete) level of compliance for success.
At the heart of the Social Navigation Hypothesis is the idea that human mood regulation operates in two overlapping modes. The first is a lowmood continuum that adaptively pulls effort away from plainly unprofitable pursuits. The second is a highgain, commitmentdevice mode—the majordepression adaptation—that engages when a person is caught in nonpointsource social entrapment. This mode coordinates a suite of responses: antilure anhedonia (suppresses attraction to irrelevant rewards), psychomotor slowdown (limits wasted effort and participation in the status quo niche), narrowed focus on the constraining relationships or institutions, costly noncooperation (raises the social price of ignoring the plight), persistence until meaningful concessions or exit occur, and significant remission that begins promptly once constraints are lifted. Such a system, while costly, provides leverage in genuine entrapment by signaling seriousness and preventing premature return to the same untenable niche; like a smoke detector calibrated to err on the side of alarm, it yields benefits in the right circumstances at the expense of more false alarms. A concise clinical summary of this sequence appears in Clarifying the common phases of the depressive sequence below.
Beyond Pathology: A Functional View of Depression
Modern psychiatry usually views major depression as a pathology—a breakdown of normal functioning. In this medical model, depression is an illness caused by genetic vulnerabilities, chemical imbalances, or brain malfunctions, with symptoms that serve no purpose other than to torment the patient. Even many evolutionary-minded scientists have assumed that while ordinary sadness might have some adaptive value, clinical depression (with its extreme lethargy,
anhedonia, and despair) must be a dysfunction—perhaps a quirk of our Stone Age brains struggling in the modern world, or an evolutionary trade-off gone wrong. This prevailing view sees nothing useful in depression’s pain.
Evolutionary psychiatry offers a very different starting point. As Randolph Nesse (2023) has emphasized, capacities for symptoms such as pain, cough, anxiety and low mood are not arbitrary flaws, but evolved defenses that were useful in particular kinds of situations. The key question, from this perspective, is not “Why do some brains break?,” but “What kinds of problems was this deeply unpleasant state built to address, and under what conditions does it become excessive or misapplied?” The Social Navigation / Niche-Change Hypothesis is one answer to that question. It does not deny that some major depressive episodes are disastrously harmful, but it asks whether others, especially those triggered by non-point-source social entrapment (logically, a complex recurring problem in traditional and modern societies), might activate a specialized defensive strategy that usually made sense in the environments where our minds evolved and, with informed interventions, may be functional in modern societies too.
Depression, anxiety, and why they travel together
Clinically, depression and anxiety are notorious for co‑occurring, and SNH actually expects that. A person trapped in non‑point‑source social entrapment is not just sad; they are living in a high‑stakes, high‑threat environment where every move can invite punishment, rejection, or escalation. In that setting, a pure “calm rumination” system would be maladaptive. The same architecture that drives analytical focus and withdrawal is likely to up‑regulate threat monitoring, vigilance, and anticipatory fear. Early and mid‑phase depression under SNH is therefore not a Zen retreat; it is a tense, effortful state in which the mind both rehearses options and tracks dangers. From a design perspective, it makes sense that genetic and circuit‑level vulnerabilities for depression and anxiety overlap: they are two arms of a broader internalizing defense package. The depressive arm slows you down, strips away non‑instrumental rewards, and forces a re‑think of your niche; the anxious arm keeps you alert to the ways your partners, gatekeepers, and rivals might respond as you push for change. Far from being a puzzle, the depression–anxiety comorbidity looks like exactly what you’d expect when a brain is trying to renegotiate its life under threat.
Proponents of SNH offer a different perspective. They point out that in biology, the costliness of a trait can itself be a sign of adaptive design. Just as the searing agony of physical pain is useful because it forces you to stop using an injured body part, the psychic pain of depression might have evolved to force a change in behavior or circumstances that ultimately protects the person. In this sense, depression’s misery could be part of its purpose rather than a sign of pure failure. It’s a counterintuitive idea: it asks us to consider that feeling awful might, in some contexts, have been better for survival than feeling okay or just mildly sad while carrying on as normal.
One of the most puzzling features of depression—its loss of pleasure or motivation, known as anhedonia—is usually treated as evidence of system failure. From a social-navigation perspective, however, this blunting of reward may itself be functional. Anhedonia can act as an anti-lure filter, temporarily suppressing the pull of non-instrumental rewards that might distract from solving the core social dilemma. By making the usual pleasures of life feel hollow, the mind reduces the chance of being “bought off” by comforts that leave the underlying constraints unchanged. In this view, depression does not eliminate motivation altogether; it reallocates motivation—discouraging effort toward irrelevant rewards (which social partners may offer with good intentions, manipulative aims, or mere cluelessness) while preserving or even heightening sensitivity to outcomes that promise genuine resolution or escape from the fitness-sapping social entrapment. This selective reward blunting predicts a measurable pattern: depressed individuals should show reduced effort for generic or symbolic rewards but normal or increased effort for rewards that directly mitigate or remove the social constraints blocking access to a better situation. In plainer terms, when someone is depressed due to an intolerable life bind, perks and pleasures that don’t solve the problem will have little effect, whereas signs of real improvement (like a concrete opportunity or support to change their life) will still stir motivation.
However, depression does not just threaten to annihilate pleasure. In more escalated cases, sufferers describe a further descent into emotional numbness or flattening—a kind of intrapsychic shutdown where they feel neither joy nor sorrow. This numbed state is akin to solitary confinement of the mind, and paradoxically, it can make the person’s plight even more alarming to observers. Although we might be surprised to hear it stated, people instinctively know that “the last thing a person will sacrifice is their suffering.” As one often under appreciated songwriter put it, “I’d rather feel bad than not feel anything at all.” 2 Embracing pain over emptiness may be a last-ditch adaptive stance: pain means one is still alive and fighting, whereas total numbness signals a dangerous collapse of meaning and engagement. In evolutionary logic, the numbness stage could be the riskiest, most extreme phase of the depressive cascade – a high-stakes gambit to spur a response when all else has failed. The sufferer has abandoned pleasure; even pain is running out; what’s left is a hollow shell that practically screams that the situation is beyond tolerating.
That sequence yields a clear prediction: if social partners respond earlier (during pain-dominant signaling), the episode should terminate before numbness appears.
Why would evolution include such dangerous elements in an adaptation? Early evolutionary thinkers about depression began to ask what possible benefits might come from such distress. Psychiatrist John Price, in the 1970s, suggested that depression after a defeat might function as an involuntary submission signal—a way of conceding loss and avoiding further conflict with a dominant rival. His “social rank” hypothesis likened certain depressions to the defeated posture of an animal that surrenders to end a fight. This explained low mood as a strategy to prevent more harm when one cannot win—essentially, “I give up; please don’t hurt me anymore.” Similarly, other researchers noted that sadness and fatigue could resemble the energy conservation seen in animals during periods of loss or winter—a kind of hunkering down until conditions improve (an idea suggested by psychiatrist Randolph Nesse in 1991). These early ideas broke from the pure “disorder” view by proposing that low mood has some function, but they usually applied only to mild cases or specific situations like rank loss. They struggled to account for the extreme features of severe depression—the total shutdown of motivation, the deep pessimism, even suicidal ideation, which on the surface seem unequivocally harmful.
The Social Navigation Hypothesis was first articulated in the early 2000s by evolutionary psychologists Paul J. Watson and Paul W. Andrews and, in parallel and independently, by evolutionary anthropologist Edward Hagen, later joined by evolutionary psychiatrist James “Andy” Thomson. Working from a different empirical starting point, Hagen’s early work on postpartum depression argued that a mother’s profound despair after birth can serve as a bargaining device—a costly, hard-to-fake way of pressing kin and partners to provide the support she needs to keep investing in a new infant. That postpartum bargaining model, published a few years before our own formulation of SNH, was one of the earliest fully developed proposals that a subtype of depression might function as a social negotiation strategy. The Social Navigation / Niche-Change Hypothesis integrates these overlapping insights about withdrawal, signaling, and the costs of unbalanced relationships, proposing a comprehensive adaptive system that links focused problem-solving, honest signaling, and the broadcasting of extortionary sanctions into a single coordinated sequence. Very much in parallel with Hagen’s bargaining model, the SNH holds that those very costs are what make the system work. In simple terms, depression is hypothesized to be so painful and disabling because, in extreme situations, shutting down ordinary functioning and making one’s suffering unmistakable may be the only way to induce others to reconsider a destructive status quo. If a person’s life circumstances are driving them—and their genetic interests—toward a cliff, a normal cheerful mood can be dangerous; a collapse into misery that halts “business as usual,” though risky and exhausting, can serve as the emergency brake that sometimes prevents even worse outcomes. It is an uncomfortable idea, but the Social Navigation / Niche-Change Hypothesis invites us to consider depression not as an error in the system but as an extreme alarm signal and last-resort extortionary mechanism that, in ancestral environments, sometimes paid off—by moving the social network in a more survivable direction—despite its terrible short-term costs.
Importantly, SNH envisions a phase-structured response. In the early phase, the depressed individual retreats socially and turns inward, dedicating heightened cognitive focus to analyze the complex dilemma (the rumination phase). Energy, appetite, and interest in trivial activities wane—costly trade-offs that free up mental resources for deep problem-solving. Many depressive bouts may resolve at this stage due successful problem-solving; this needs more testing. If this introspective phase fails to yield a solution or if the individual alone cannot effect the needed changes, the social-signaling phase intensifies. Here the symptoms (e.g. profound fatigue, despair, even suicidal expressions) function as costly signals that broadcast the severity of the impasse. Close partners and kin, who have a stake in the depressive’s welfare, are thereby pressured to help resolve the issue or make concessions – a dynamic sometimes described as honest signaling or passive extortion. The regulatory logic of SNH is that depression’s intensity adjusts to context: it escalates when vital needs are unmet or social partners are unresponsive and abates once the underlying problem is alleviated. In other words, the duration and severity of an episode are not random – they are calibrated to persist until either the person’s life niche changes for the better or the effort proves futile. This perspective explains why depression can spiral dangerously if relief never comes, yet can remit rapidly when a breakthrough occurs (for example, escaping an abusive environment or finally obtaining a crucial resource).
SNH predicts that depressive states tend to improve when sophisticated nonconscious regulatory systems register that concrete progress toward changing the social niche is underway (see Concession/Exit measure below). The hypothesis predicts that improvement in such cases should track the occurrence of verifiable concessions or exits that alter the person’s social constraints—changes in workload, authority, resources, living arrangements, and so on. We can refer to this as the Concession/Exit measure, because it operationalizes “niche change” in terms that can be observed and counted. In principle, one can test the Social Navigation / Niche-Change Hypothesis by asking whether symptom relief in depression is specifically tied to these documented, constraint-altering outcomes, rather than to generic support or simply the passage of time.
When should relief begin? Notably, SNH does not claim that depression only lifts after a life problem is fully resolved. Rather, it predicts that symptoms will often start to ease as soon as the mind detects real momentum toward a solution. For example, if concrete steps have begun—training for a new role, moving out of an oppressive home—and key social partners have made binding, instrumental commitments to help those steps, the depression should begin to soften. In other words, the trajectory should improve when credible progress is in motion, not only at the end point. This yields a straightforward, testable prediction: mood and functioning should track leading indicators of niche change (such as scheduled renegotiation meetings, signed agreements to shift roles, funded training or relocation plans, or documented changes in who does which work and who controls which resources), and should do so more strongly than they track generic encouragement, medication, or time passing. In short, progress that truly moves the niche should move the mood most.
Prolonged depression as chronic thwarted niche change. In modern societies, however, the conditions that originally call up the high-gain depressive response often do not shift in the way the system “expects.” A soldier may return from a tightly knit combat unit to a fragmented civilian setting that cannot absorb his skills, offers little acknowledgment or shared purpose, and provides only thin bureaucratic support. A parent in a precarious service job may know exactly what changes would make life livable—secure childcare, a reliable income, a less abusive supervisor—yet find that every door is bolted from the other side. In such contexts, the depressive system can continue to press for niche change, but the partners and institutions it is trying to move remain immobile. From the outside this looks like “chronic,” “non-responsive,” or “treatment-resistant” depression. From an SNH perspective, much of this chronicity is not evidence that the adaptive machinery has “gone wrong,” but that it is trapped in an extended, losing campaign: a prolonged, costly bargaining stance sustained because the underlying social impasse never resolves. The distress is real and often life-threatening, and it must be treated; yet the conceptual point remains that an adaptation can look pathological when it is run in a world that offers no way to do the job it evolved to do.
Modern mismatch and thin ties. In small, tightly knit groups, a neighbor’s distress is hard to ignore: the wail of a child, the slumped posture of a hunter who has failed repeatedly, the woman who stops coming to the fire at night. Those cues typically draw real, costly help because everyone’s fortunes are entangled. By contrast, modern social life surrounds us with hundreds of shallow ties and a constant stream of curated signals on screens. We may accumulate thousands of “friends” and “followers” without having more than a handful of people who will actually lose sleep or money to help us solve a serious problem. Under those conditions, even relatively ordinary setbacks can feel like social abandonment. The low-mood system that evolved to register “no one is helping” gets triggered more often, and its early phases—sadness, moping, minor depression—have less chance of being interrupted by genuine partner commitments. In short, the problem is not that modern life is “too hard” in brute-force terms; it is that our social ecologies maximize apparent contact and minimize the kind of costly commitment that produces real concessions or exit. Where authentic, binding commitments are rare, those early phases of depression are more likely to consolidate and escalate toward the high-gain, major-depressive mode instead of resolving quickly.
Testable prediction (preview for Essay 2): As the ratio of weak‑tie to strong‑tie relationships rises, early‑phase sadness and minor depression should be more frequently precipitated by modest setbacks, because more of those setbacks will be experienced as unshared burdens.
By contrast, a generic “dysregulation” view of depression would predict a more indiscriminate pattern: any uptick in expected reward (social or nonsocial) should brighten mood. The SNH view is more specific: in depressions precipitated by non-point-source entrapment, symptom relief should be disproportionately tied to actual social resolution—to verifiable concessions or exits and the concrete commitments that lead to them. Generic support or passing time may help somewhat, but after controlling for their effects, improvement should track those constraint-altering changes much more strongly. In other words, if someone’s depression really is an evolutionary “alarm” about a bad life situation, then solving that situation (or demonstrably starting to solve it) should correlate with them getting better, far more than simply receiving comfort or waiting it out.
We will explore in a separate essay the empirical agenda needed to fully test these predictions. But even now, we can see hints of this pattern in everyday life—for instance, a depressed new mother’s mood often lifts rapidly once she’s given genuine support with childcare, not just pep talks. That is exactly what SNH would predict.
Readiness and capability-building. It’s important to clarify that SNH does not imply a depressed person is automatically ready to step into a brand-new life the moment others concede or offer help. Often where an inadequate outgrown niche creates a mismatch between a person’s capacity for major increases in their fitness-enhancing activities, but their opportunity to do so is blocked by complex social constraints, the person may need training, practice, or new resources to enable them to thrive in that better niche. The appropriate strategy in therapy, therefore, is to convert that gap into a concrete plan. For example, if someone is depressed because they feel stuck in a dead-end role, effective help would involve setting up skill-building or retraining opportunities, reallocating some of their time away from non-instrumental duties that merely maintain the untenably low return on investment status quo niche, and securing commitments from partners (e.g., for childcare coverage, introductions, financial support for courses, etc.) that make the transition feasible. In SNH terms, even preparatory steps count as progress: nonconscious valuation and control systems are sensitive to credible momentum toward change, not only final end‑states. In practice, the convener (therapist/mediator/supporter) should make legible and reinforce enabling steps—enrolling in a class; a spouse making a dated, written commitment to take over specific chores—because these are precisely the signals of change a depressed person’s mind is tracking.
After neural injury, the same logic holds, but the executive–affective interface may be partially compromised. In such cases the convener’s role becomes even more critical: externalize planning, scaffold partner commitments, and keep progress legible (checklists, calendars, receipts, shared dashboards) to the systems that regulate mood. SNH mechanisms are likely to be engaged whenever circumstances demand niche change and/or sustained new forms of costly social support; they can be applied while acknowledging substrate limits from injury and adapting goals to residual capacities. (Scope: where depressive episodes lack a salient social‑constraint problem, SNH predictions may not apply.)
Many evolutionary psychiatrists have argued that negative emotions such as low mood are best understood as evolved defenses rather than arbitrary defects. Building on that general point, the Social Navigation / Niche-Change Hypothesis makes a more specific, testable claim: in the subset of episodes produced by non–point-source social entrapment, the high-gain mode of low mood functions as a coordinated negotiation system—one that integrates analytical rumination, honest signaling of need and commitment, and, only if those fail, last-resort sanctions that withdraw benefits from unresponsive partners. On this view, bargaining and sanctioning are built on a foundation of honest signals: the individual must credibly communicate both that their situation is unsustainable and that they are prepared to move into a different niche if others will help. The defensive state should therefore remit preferentially when verifiable concessions or exit are underway, because at that point the information-gathering and signaling goals of the system have been met.
The Three Functions of Depression: Problem-Solving, Signaling, and Sanction
According to the Social Navigation Hypothesis, depression operates via a triad of functions that work together to help a person stuck in an untenable situation. First, depression focuses the individual’s mind inward on the core problem (intensive rumination). Second, it sends an honest signal of need to others through visible distress. Third, if those two steps do not resolve the issue, depression withdraws the person’s contributions to others—essentially imposing costs or sanctions on the social partners who are maintaining the status quo. (For how these functions typically unfold across stages, see “Clarifying the common phases of the depressive sequence” below.)
How SNH differs from generic sadness dysregulation. A general dysregulation view holds that subclinical low mood downshifts effort when expected returns are poor and improves after any increase in expected value—social or nonsocial. By contrast, the Social Navigation account is specific: in episodes precipitated by nonpointsource social entrapment, symptom relief should be disproportionately tied to social resolution—verifiable concessions or exits—and to binding partner commitments that cause those steps. Generic encouragement, medication, or time may help, but after controlling for magnitude, improvement should track the constraintaltering changes recorded in the Concession/Exit measure more strongly than it tracks nonspecific factors (see Concession/Exit measure below). The same discriminating prediction applies in injury cohorts: remission should align more with documented social concessions/exit than with generic support or time—even though circuit damage may blunt the magnitude or tempo of response. In short: progress that moves the niche should move the mood most.
When persuasion and honest signals of need do not yield change, the same system escalates from plea to sanction: the sufferer’s capacity collapses and their ordinary contributions are withdrawn—an involuntary “strike” that imposes costs on partners who maintain the status quo. The credibility here does not come from words but from costliness: psychomotor slowing, pervasive anhedonia, and functional withdrawal are hard to fake and expensive to endure. This is not conscious manipulation; it is a nonconscious regulatory shift that pressures gatekeepers to concede or enable exit. The core prediction is correspondingly concrete: early, visible noncooperation should cooccur with—and predict—rising partner concessions, and symptom relief should track those concessions or binding commitments; absent movement, escalation toward numbness and parasuicidality becomes more likely. Hagen’s bargaining model captures the same logic with the laborstrike analogy; our “fitness extortion” language makes the leverage explicit.
We will examine each of these in turn.
Focused Rumination: Depression as Intensive Problem-Solving
One facet of depression’s potential evolutionary function is a distraction resistant, problem focused mode often called analytical rumination. When someone faces a major life dilemma—say, loss of status, an exploitative relationship, or a sudden new burden they cannot handle—it can be useful for the mind to pull back from normal life and focus, often to the point of obsession, on the problem. Such situations can render the person’s current socioeconomic niche unsustainable: no longer a good way forward for maximizing lifetime inclusive fitness, every organism’s ultimate—if nonconscious—raison d’être. Positive developments can create the same mismatch (for example, a credible opportunity to develop a lucrative skill or launch a promising idea that the current niche cannot support). In contemporary systems language, this looks a lot like rootcause analysis: the mind keeps returning to the question “What is the deeper pattern that keeps recreating this mess?” rather than only “How do I get through tomorrow?”
In such contexts, depressed mood often supplies the rumination required to plan negotiation strategies and to build support for major niche revisions. It narrows attention, drives a relentless inward focus on the constraint set, and devalues hobbies, sex, and other distractions. The aim is not just to replay hurts, but to decompose the tangle into subproblems—who controls which resources, which obligations can be dropped, which alliances could be reconfigured—and to search for levers that make a better niche reachable. Think of the movie Groundhog Day (how great is Bill Murray?). Yes, things are replaying. But each instance is used to devise a better outcome. That is exactly what should be happening whenever replays are a major feature of depressive analytical rumination.
Recent work shows that when rumination is measured properly - that is, in a way that reflects its proposed function rather than its surface phenomenology - depressive cognition exhibits the structured, problem focused dynamics predicted by analytical models. In a large, multi-sample study spanning clinical and non-clinical populations, Bartoskova et al. (including Paul W. Andrews) showed that depressive rumination is not a single undifferentiated blob: it can be decomposed into analytically distinct components (especially causal analysis and problem-solving analysis) that covary with depressive symptoms in a patterned way. In that same line of work, the authors also introduced and validated a theory-driven instrument for measuring analytical rumination (the Analytical Rumination Questionnaire), designed specifically to distinguish causal analysis and problem-solving from more generic “brooding” - allowing direct empirical tests of functional predictions that standard rumination scales can obscure.
In real life, depressive rumination rarely operates in isolation. Once visible suffering and withdrawal are in play, other people do not just provide comfort; they start trying to figure out what to do. A central claim of the Social Navigation / Niche‑Change Hypothesis is that this is part of the adaptation, not a side effect. The depressive sequence is built to recruit other brains into the problem: family members, partners, and key allies are drawn into offering diagnoses (“Here is what’s really wrong”), strategies (“Here is how we could change this”), and concrete niche‑building help (money, housing, introductions, workload shifts). In that sense, depression is a way of forcing a whole small network to run a joint search for a better life arrangement. The sufferer’s own rumination is only Stage One of that process. The honest signaling of need and, if necessary, the involuntary “strike” that withdraws their usual contributions are the levers that buy access to others’ cognitive and practical resources. On this view, the unit of adaptation is not a solitary thinker optimizing their plans, but a bargaining campaign that recruits a coalition to help redesign and implement a new niche.
While this withdrawal and brooding feel terrible and, at high levels, can even be debilitating, the hypothesis is that their function is to force a person to confront the source of distress—perhaps even penetrating to its root cause—with prolonged full focus. Under SNH, the key driver is an unusually stubborn lack of all the necessary social support for a significant step toward a better niche—as if the mind declares, “This issue is so important you cannot do anything else until you understand what caused it and what must change.”
There is some evidence that mild depression or sadness sharpens certain kinds of thinking. Studies of “depressive realism” observe that mildly depressed individuals sometimes make more accurate judgments about self and control than nondepressed people, who often show optimistic bias. In everyday life, a mildly depressed person may appraise relationships or failures more soberly, whereas a cheerful person might gloss over real problems. From an evolutionary perspective, seeing reality more clearly—even when it hurts—could help recalibrate strategy. Low mood in this respect forces a sober and relatively detached review of recent losses, threats, and mistakes to glean actionable insight.
Importantly, this cognitive/problemsolving function is most plausible in mild to moderate depressive states (demoralization or prolonged sadness) where the person can still think relatively clearly. In major depression, as the episode deepens, cognition often deteriorates—memory and concentration falter, decisionmaking feels impossible, and the mind can spiral into hopeless thoughts. ³ Even granting that decline, the SNH reading stays coherent: the analytical “problemsolving” mode is the opening act. If a person cannot find a solution on their own, the same syndrome shifts gears into social functions: first an honest signal of need, and—if persuasion fails—an involuntary “strike” that withdraws ordinary contributions to raise the cost of maintaining the status quo. This sequencing explains why the most disabling symptoms—profound fatigue, marked psychomotor slowing, and suicidal ideation—cluster in more severe depression: by that point the aim is no longer to think your way out, but to force change with the help of others. ⁴
Honest Signaling: The Depressive “Cry for Help”
When personal analysis and rumination cannot fix the problem, depression appears to activate a strategy of social signaling—recruiting assistance by broadcasting need and incapacity. A depressed person’s behavior (sobbing, withdrawal, loss of appetite, exhaustion) is hard to fake and costly to sustain, which makes it an honest cue that something is seriously wrong. In small, interdependent groups, such signals often elicited concrete, costly aid; ethnographic and clinical observations suggest this is especially visible in burdens like the postpartum period, where depressive symptoms can operate as a bargaining signal for additional support from partners and kin, with relief tracking the provision of sustained help. In that sense, depression is not simply “expression of distress,” but a move in a social negotiation: it raises the salience of unmet obligations, invites redress, and—if ignored—sets the stage for more forceful tactics later in the sequence.
In the small, interdependent social groups of our ancestral past, such a signal would not only be noticed but often lead to assistance. Humans are cooperative creatures, especially toward family and close friends. If a group member became non‑functional and obviously miserable, it would alarm the others. It is as if the behavior says, “I can’t cope with this situation—I’m overwhelmed.” Under the SNH, this is step one of depression’s social strategy: invite help by being visibly in distress. Often this can prompt a quick resolution. Postpartum depression (which affects roughly one in seven new mothers) is an especially clear case: it can operate as an honest signal that a mother is overburdened and needs more support, and observational studies show that stronger postpartum symptoms are often followed by increases in childcare support from partners and kin, with mood improving as that help stabilizes. Recent experimental work by Edward Hagen and colleagues goes further, using vignette studies to show that when observers see a victim in conflict who responds with depressive collapse or suicidal threats, they judge that person as more genuinely needy and truthful and feel more obligation to help compared to otherwise similar cases without such cues. In other words, third parties spontaneously treat depressive and self‑harming behavior as credible signals of need, not as random noise—which is exactly the pattern SNH predicts for an honest, fitness‑relevant “cry for help.”
Gaffney, Adams, Syme, and Hagen (2022) provide one of the closest things in the literature to a direct experimental test of the core proximate claim: that depression-like impairment and, at the extreme, suicidality, can function as a socially legible, credibility-enhancing signal of need in conflicts of interest.
They used preregistered experimental vignette studies in which participants occupied the role of a potential helper or decision-maker facing a dilemma where the claimant had incentives to exaggerate and where the truth of the claimant’s need was private information. Participants first rated (i) how much they believed the claimant and (ii) how likely they would be to provide help. They then learned that the claimant displayed one of several signals that differed in “cost”, in the sense of reducing productivity or putting future productivity at risk: a simple verbal request (control), crying, mild depression symptoms, depression symptoms, or a suicide attempt. Importantly, the vignettes described symptoms and the attempt rather than leaning on diagnostic labels (they did not rely on the words “depression” or “suicidal”).
Across vignettes, as signal cost increased, both belief and willingness to help increased in the predicted rank order, with the largest shifts for depression and a suicide attempt. The key theoretical point is not merely that people “feel bad” and want to help, but that the costly signals changed what observers inferred about credibility and need. Consistent with an honest-signaling logic, the effect of the signals on willingness to help was largely mediated by increased belief that the claimant’s need was genuine. In pilot work, the authors also tested (and rejected) a simple “any psychiatric distress triggers sympathy” alternative by including a condition in which the claimant displayed schizophrenic symptoms, which produced dramatically lower belief and willingness to help than any other condition.
This study shows something crucial for the positive case: in contexts where there is a conflict of interest and suspicion is rational, depression-like impairment and suicidality are treated by observers as higher-credibility signals than verbal requests, sad expressions, or tears, and they can shift stated cooperative intent in the predicted direction. Vignette responses are not real-world behavior and MTurk samples are not representative, but randomized manipulation, preregistration, and cross-cultural sampling make this evidence unusually diagnostic for the “social leverage via legible costly signaling” premise.
Neurobiological work on postpartum depression adds a useful proximate layer to this picture. During pregnancy, levels of certain hormones and “neurosteroids” rise dramatically and then crash after birth; in some women, this abrupt drop appears to destabilize brain circuits that use a calming chemical called GABA. New fast‑acting drugs such as brexanolone and zuranolone temporarily restore that neurosteroid tone and can sometimes lift postpartum depression within days rather than months. That is a genuine mechanistic advance: we are learning how to reset, pharmacologically, a mood system that has been driven into an extreme defensive state. From an SNH perspective, though, this does not replace the functional story; it sits alongside it. The evolutionary question remains: which mothers are pushed to the point where that system fires so hard, and under what support conditions? A pill that steadies GABA‑sensitive circuits can make a mother feel like herself again—and that is worth celebrating—but it does not, by itself, change whether she is still trying to raise an infant in an overburdened, under‑supported niche. The biology explains how the alarm can be switched off; SNH still asks why the alarm was activated in the first place.
This honest-signaling phase of depression can be seen in plenty of modern examples. A normally reliable employee who falls into a funk may (unwittingly) be sending the signal that they are overworked and need a break or assistance. A student who becomes depressed after a humiliating social incident might be indirectly signaling to friends and family that they are deeply hurt and in need of comfort and reassurance. In all these cases, the depressive behaviors communicate a clear message without the person deliberately choosing to send one. Much like a baby’s wail or a wounded person’s cries, it’s an instinctive expression of distress. If those around respond with care, concessions, or problem-solving, SNH predicts the depression should abate – its job is done.
In a world where most interactions are with weakly committed partners, the honest signals of need that depression sends may be seen but not acted upon. A hundred thumbs‑up icons are not the same as one neighbor showing up with a casserole or offering to watch your kids. To the nonconscious systems that regulate mood, both the absence of costly help and the presence of perfunctory, low‑effort responses register as “no one really has your back”—precisely the situation in which sadness, and in more extreme cases major depression, are most likely to emerge.
Honest signals needed on both sides. Of course, a sufferer’s need alone rarely moves others unless it is met with credible commitment from those others. In the social-navigation view, the depressed person’s suffering communicates need, but progress depends on reciprocal signals of commitment from the people who control access to a better niche (the “gatekeepers”). These commitments must be costly to fake, specific, and binding to truly count. Examples include: a formal change in someone’s role or workload put in writing; a concrete reallocation of resources or authority; agreed timelines for safety or policy changes; or tangible assistance with exit steps (e.g. providing childcare coverage, writing a job reference, offering temporary housing). Empty reassurances or vague “we care about you” sentiments do not suffice – actions are required. The hypothesis predicts that earlier, stronger partner commitments will lead to faster and more complete recovery, because they pave the way for real concessions or escapes, over and above the effects of generic sympathy or even medication. (In other words, if key people step up and prove by their actions that help or change is coming, the depression should begin to lift, whereas if everyone just says kind words but nothing actually changes, the depression is likely to persist.)
The therapist as convener. In modern settings, a skilled therapist, counselor, or mediator can sometimes act as a convener – helping translate the depressed person’s signals into actionable commitments on both sides. In practice, this means the therapist might work with the patient to articulate what they need (and what they themselves are committed to doing) and then facilitate conversations or agreements with the relevant family members or institutions. For example, the therapist can help the patient identify and communicate their own honest commitments toward change (e.g. “I will refuse unhealthy temptations; I will apply to new jobs; I will set clearer boundaries”), and then convene the family or other partners to secure parallel commitments from them (e.g. “We will hire a babysitter twice a week,” or “I, the employer, will reduce your workload for the next month”). Because severe depression can make it hard for the person to advocate for themselves, the convener essentially speaks for the depressive signal: asking concrete, low-ambiguity questions (“What would real progress look like by next week?” “Which current obligations feel unbearable?” “What change from your partner would ease this feeling?”) and translating the answers into clear actions with deadlines. The convener’s goal is not to cheer the person up in the moment or try to convince them that their “negative” thought patterns are unwarranted, but to shepherd visible, meaningful changes that the person’s deep mind can recognize as the alleviation of their plight. In SNH terms, the therapist is helping to generate the honest commitments and concessions that the depressed brain is waiting for. When clear, costly help is not forthcoming from those who control the constraints, the same system escalates.
Involuntary Withdrawal: “Fitness Extortion” and Social Sanctions
Note that the experimental vignette evidence summarized above most directly supports a belief-updating, honest-signaling channel: costly depressive signals change what observers infer about credibility and need, which then changes willingness to help. The extortionary “strike” or cost-imposition channel discussed next is conceptually distinct: partners blocking niche change may also shift behavior because the depressed person’s withdrawal imposes costs on them, even when it does not materially change their private beliefs about the underlying dispute that honest signaling of need could bring about.
If honest signaling and selfproblemsolving fail, depression escalates by withdrawing the person’s contributions and participation—an involuntary “strike” that imposes costs on partners who benefit from the status quo. This is not a chosen tactic; it is a nonconscious sanction that makes businessasusual impossible until concessions or exit open the path to a better niche. The sanction phase functions as leverage: it raises the price of ignoring the sufferer by reducing productivity, warmth, reliability, and availability, sometimes progressing to psychomotor collapse and emotional flattening. In SNH terms, this is “fitness extortion” in the strict evolutionary sense—the system withholds benefits to force renegotiation—and it relaxes abruptly once constraintaltering commitments or exits are credibly in motion.
It’s critical to understand that this is not a calculated ploy or a message in the normal sense. The person isn’t faking illness to manipulate others – they are genuinely incapacitated. However, the effect of this incapacitation is that it imposes costs on those who depend on the depressed person. If a mother or father “shuts down,” the rest of the family loses a caregiver. If a worker stops functioning, the employer and colleagues lose productivity. If a friend completely withdraws, the social circle loses that person’s contributions. In our ancestral groups, losing a member’s participation – even temporarily – could be a serious blow to survival, since tasks like hunting, gathering, child-rearing, and defense were cooperative endeavors. Depression in this view is analogous to a labor strike: when one member of a tightly knit group stops contributing, everyone feels the strain.
Why would evolution favor such a drastic, self-harming strategy? Because sometimes leverage is needed to force a renegotiation. If a person is stuck in a harmful situation that they cannot exit or change alone, and if those with the power to change it are reluctant to do so (perhaps because change would cost them something), then making those others feel some pain too might be the only way to get movement. It’s a dangerous gambit – much like striking workers sacrifice wages, a depressed individual “on strike” sacrifices their ability to function and feel pleasure. But if the status quo is untenable, enduring short-term pain could lead to a better long-term outcome once a new understanding is reached.
Evolutionary anthropologist Edward H. Hagen, who helped develop this bargaining model of depression, explicitly uses the labor strike analogy. He notes that a strike hurts the strikers, but they undertake that pain because continuing under the current conditions is even worse for them. By withholding their labor, they force “management” (others in the group) to come to the table. Similarly, a depressed person’s involuntary withdrawal of effort and engagement can force previously uncooperative partners to finally pay attention and negotiate. Think back to our earlier example of the ignored elderly man: if his initial expressions of sadness and loneliness don’t prompt his family to include him, his depression may deepen to the point that he stops trying at all. He stays in bed, shows no interest in anything, maybe even hints at not wanting to live. This imposes an emotional and practical burden on the family – they feel the gloom in the household, they have to manage tasks he once did, and they might worry about his survival. In effect, his depression is making his absence felt in a very tangible way. If the family members have any attachment or rational interest in him, this cost gives them a strong incentive to change their ways (for example, to actively bring him back into family activities, seek his advice, reassure him of his value). When they do make those changes and improve his social niche, SNH predicts the depression will resolve – just as a strike ends when management and workers strike a better bargain.
Both the honest signaling and the extortion phases of depression are involuntary and costly, which is exactly what gives them credibility. The depressed person isn’t choosing to “punish” anyone – it’s an automatic collapse. But, in evolutionary history, those who responded to such collapses with help and concessions may have been more successful in keeping valuable partners (or kin) alive and eventually well. Conversely, ignoring depression in a group member could mean losing them entirely (through suicide or permanent disability) – a loss that would also harm those left behind. So our ancestors may have been shaped to pay attention and try to relieve the causes of a group mate’s depression, because doing so was in everyone’s genetic interest. This dynamic could make depression an evolutionarily stable strategy under certain conditions: if you are trapped in a bad situation, becoming depressed will either elicit help from your network or impose costs until they relent, and in the long run either outcome is better (for you and your genes) than silently bearing a situation that is destroying your fitness.
It must be emphasized that describing depression in these strategic terms does not imply any conscious manipulation by the sufferer. A person with major depression is not plotting or scheming to gain advantage; they usually feel utterly helpless. The “strategy” we are talking about is encoded at the level of emotional reflexes and behavioral tendencies, shaped over millennia. That is, nonconscious control systems are in charge. Just as an infant doesn’t plan to cry for milk – it just cries and thereby gets fed – a depressed adult doesn’t decide to withdraw to punish others; it just happens as a result of the depressive process. The intentionality is evolutionary, not individual. Understanding this can actually foster compassion: the person’s extreme pain and dysfunction is not their fault or under their full control, yet it may be serving a desperate purpose when viewed through the long lens of adaptation.
Clarifying the Common Phases of a Depressive Episode
The picture that emerges is not of a single “sadness knob” that simply gets stuck on high, but of a specialized configuration of the lowmood machinery tuned to a very particular kind of predicament. In everyday life, when plans go sideways, humans rarely need a mood state to declare that “effort is futile”: the usual response is to try something different, enlist allies, and improvise. The Social Navigation / NicheChange Hypothesis addresses what happens when those ordinary strategies fail. In non–pointsource social entrapment—where vital goals are blocked by a tangle of obligations and by partners who will not or cannot help—low mood can shift into a highgain mode whose job is not to conserve energy but to restructure a failing social niche. In that mode, the mind first locks onto the entrapment problem with compulsive rumination, then progressively devalues noninstrumental rewards, then makes suffering and incapacity increasingly visible to others, and only in the later stages recruits more global fatigue and flattening. On this account, the escalation we call major depression is not random “decompensation” but a sequenced attempt to solve a deeply social problem—by forcing recognition, renegotiation, or, if necessary, exit from an untenable life arrangement.
Where social partners respond early to honest signals of need, the process should deescalate after the initial phases; where they do not, the same adaptation can drive the organism into more extreme, outwardly catastrophic stages. SNH applies across intensities: it describes depression as a graded response that can escalate through a sequence of stages if the underlying social problem remains unresolved. It therefore calls into question reflexes to pathologize a person’s episode as “chronic,” “nonresponsive,” or “endogenous” in the absence of evidence that the constraining social matrix has actually changed.
In parallel, improvement should track documented concessions or exits—the concrete alterations in workload, authority, resources, or living arrangements that signal real movement toward niche change.
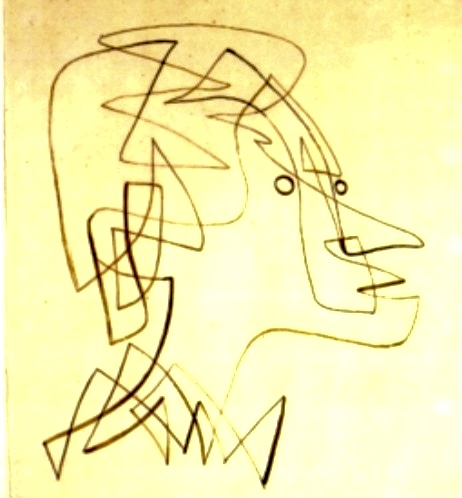
Before going further, it’s worth clearing up a common confusion about rumination. Not all rumination is the same beast. Some of it is abstract and existential—‘What kind of life am I living?’ ‘How did I end up here?’—and some of it is concrete and tactical—‘Who controls what?’ ‘What can actually change, and how?’ In depression, the mind often starts in the abstract mode, because first it has to loosen its grip on a life that may still contain comfort, loyalty, and things worth loving, but no longer works. Only after that detachment can it move on to practical planning. Trouble arises when the mind gets stuck circling the abstract questions and never lands on actionable steps, usually because the social environment has not yet made concrete movement possible. That’s not evidence that rumination is useless; it’s evidence that the transition failed. The details matter.
Interestingly, this distinction between existential, meaning-focused rumination and later tactical problem-solving has long been explored in literature and film - often more clearly than in the clinical literature. Artists have repeatedly portrayed characters who must first detach from who they were before they can plan who they will become. (Many readers will think of particular songwriters or actors who have made careers out of portraying this sequence.) We return to this idea in Appendix A.
These stages correspond to the functional ‘modules’ we’ve just discussed (rumination, signaling, sanction), typically unfolding in order although they can overlap. A typical progression might look like this:
- Stage 0: Entrapment trigger & expected-value-of-control downshift (the “gate”). Even before what we’d call a full depressive episode, the person encounters a socioeconomic inclusive fitness entrapment (a very complex social bind or unsolvable social dilemma). In response, their brain automatically downshifts the expected value of expending effort working within the confines of that contractual matrix. This reduces motivation to act, willingness to exert effort, engagement with tasks, and persistence – especially regarding activities that are irrelevant or low-instrumentality for solving the core entrapment problem. In plain terms, the person starts to “give up” on things that won’t fix their situation. This Stage 0 looks like growing demoralization or fatigue. It’s not yet depression, but a pre-depressive state, perhaps one of significant discouragement, where, for example, an overworked employee stops striving for employee-of-the-month, or an unappreciated spouse stops going out of their way to please others. A modern term for it might be ‘quiet quitting.’ Importantly, SNH frames this not as a global malfunction, but as a selective withdrawal of effort: the mind is conserving energy for the real problem.
- Stage 1: Compulsive, focused rumination. The person’s thoughts become increasingly consumed by the dilemma, producing more cognitive effort directed at the niche-change problem. They may replay events, imagine confrontations, or devise strategies nonstop. The function here is to adopt a more sober, realistic view of their current social niche versus the alternatives, stripping away rosy illusions. The mind tries to pinpoint what specific changes or negotiations might improve things, and whom to target with these appeals. In effect, Stage 1 corresponds to the analytical rumination function described earlier.
A key reason depressive rumination has been widely treated as maladaptive is methodological rather than theoretical. Most studies rely on generic rumination scales that conflate qualitatively distinct processes (such as self-critical brooding, causal analysis, and solution generation), thereby obscuring the very dynamics analytical models predict. When rumination is measured with instruments designed to capture its proposed functional subcomponents, especially separating causal analysis from solution-generation, depressive cognition shows a replicable two-stage structure rather than an undifferentiated “brooding blob.” This helps explain why generic rumination scales often make depression look cognitively useless: they confound the very processes analytical models predict with forms of self-attack that are more plausibly byproducts or derailments. When theory-derived measures that separate causal analysis from problem-solving are used instead (e.g., the Analytical Rumination Questionnaire; Andrews & colleagues, 2014), depressive cognition shows the mentioned structure in which elevated symptoms covary with intensified analysis, and symptom trajectories are more consistent with that regulated analysis-and-stand-down process than with a simple ‘rumination is toxic’ story.
- Stage 2: Escalating anhedonia. The person experiences a deepening loss of interest or pleasure in almost all ordinary activities. This serves as an anti-lure filter: it reduces participation in the status quo and in go-along-to-get-along social rituals. The lack of pleasure is itself costly and highly visible, which helps signal to others that something is very wrong. Biologically, pleasure circuits down-regulate to prevent distractions or “buy-offs” from the core problem. The person’s lack of interest in routine rewards means they become less productive and less responsive to everyday incentives, which lowers their immediate fitness or efficiency. However, they still feel pain and urgency about the unsolved dilemma. The function of Stage 2 is to sharpen focus (by blocking out trivial satisfactions) and to begin honestly signaling need. It also reduces even further any “rose-colored glasses” attachment to their current socioeconomic life, making it easier for them to contemplate a dramatic change. (Stage 2 is essentially the onset of the honest signaling function—pain without distraction.)
- Stage 3: Pain-dominant signaling, where things typically ‘go clinical.’ At this point, psychic pain becomes intense and overtly expressed. The person may cry often, verbalize despair, or show agitation. This is the classic “depressive distress” that broadcasts need and can evoke concern and help from observers. Suicidal thoughts or gestures (parasuicidality) often kick in here as well, which, from SNH’s perspective, further underline the seriousness of the threat. The function of Stage 3 is to provide a very hard-to-ignore honest signal of need and crisis, enhancing the credibility of the plea for help. (Stage 3 corresponds fully to the honest signaling phase discussed above, and it often overlaps with Stage 2.)
- Stage 4: Energy collapse (psychomotor slowdown). If adequate help or change still isn’t forthcoming, depression may deepen into a state of profound fatigue and slowing. The person can barely get out of bed; even basic tasks feel impossible. This enforces a kind of involuntary non-cooperation: it becomes physically difficult for them to keep “playing along” with the old demands. From an SNH viewpoint, this is where the extortionary aspect really takes hold – the depressed individual’s incapacity itself starts to impose costs on others. The function here is to sanction unresponsive partners: if gentle signals didn’t work, now the person’s utter collapse presses the issue by making it impossible for the social system to continue as normal. (Stage 4 is an escalation of the fitness extortion phase.)
- Stage 5: Emotional flattening and possible catatonia-like shutdown. This is the ultimate escalation of depression’s sequence. The person’s affective and motivational systems nearly shut down. They might become emotionally unreactive, stare into space, or even slip into a catatonic-like state. At this point, nothing moves them. They may report feeling effectively nothing (not even anguish, just emptiness). In SNH, this is the last-ditch effort: “If nothing moves you when I’m in agony, perhaps you’ll move when I’m empty.” The display of utter incapacity may finally trigger a last-resort social intervention, because the alternative apparently might be the person’s death. This stage is extremely costly - it risks the person’s life and health - but it can still increase the probability of rescue or a negotiated solution if anything can. Parasuicidal behaviors, self-harm or dangerous actions that stop short of suicide, and even genuine suicide attempts are most likely at this stage. The function of Stage 5 is to further escalate the pressure on those social partners who still find it in their interests to block niche change or other problem-solving in spite of having received the depressive’s honest signals of need. Here, the depressed person has been pushed beyond pain into a state of living death, indicating that, for them, the social impasse is utterly unsustainable. This is the extreme end of the fitness extortion phase.
Note: These stages aren’t perfectly distinct steps; they can co-activate or skip around. The ordering is probabilistic, not rigid. Nevertheless, this staging highlights a logical progression in depressive episodes. And it yields a clear prediction: if social partners respond earlier (for example, during the pain-dominant Stage 3), the episode should resolve before the later, more dangerous numbness of Stage 5 ever appears. In short, the sooner meaningful help arrives, the shorter and less severe the depression should be.
When the Alarm Sounds – Triggers for the Depressive Strategy
What kinds of life situations tend to activate this drastic social-navigation system? Research and clinical observations suggest that depression most often follows events that destabilize a person’s social position or reveal that their current life “niche” is unsustainable. In simpler terms, depression hits when something about the person’s role in their world becomes unviable and needs reforming.
Negative life events are the classic triggers. These include things like: the death or departure of a spouse or loved one; a humiliating defeat or loss of status (such as being fired or publicly shamed); the loss of material resources or livelihood; being trapped in an abusive or exploitative relationship; or becoming overwhelmed by caregiving or work burdens with no relief in sight. In such scenarios, a person often experiences intense feelings of helplessness or entrapment, which psychological studies have found to be strong predictors of depression onset. If you feel “there’s no way out” of a bad situation, that is precisely the condition where shutting down might be the only way to signal distress and force a change. In fact, John Price’s early “rank theory” zeroed in on loss of social status as a key trigger: a major defeat can set off depression. SNH embraces that but adds that it’s not just the loss itself – it’s the cascade of broken social contracts that follow the loss. For example, losing a job isn’t only a blow to pride; it also disrupts one’s entire network of obligations and support. Allies at work may drift away, bills pile up, family roles get strained. Depression in such a case can be seen as a process that forces a comprehensive reorganization of one’s life when incremental adjustments aren’t enough. The person may need to establish a new identity, seek new allies, or renegotiate duties with their spouse – all big changes that others may resist. Depressive withdrawal in this context essentially says, “I can’t carry on under these old terms.”
Interestingly, positive life events can also trigger depression if they overload the person beyond what they feel able to manage. Evolutionary psychiatrists have noted that even seemingly happy events – a big promotion at work, getting married, having a baby, sudden success or fame – can precede depressive episodes when those events create new pressures or expectations that the individual cannot fulfill. For instance, imagine someone promoted to a higher-status job which on paper is a triumph, but privately they realize it demands skills or hours that will wreck their family life or exceed their capacities. The conflict (stay in the new role and flounder, or step down and feel like a failure) may be hard to resolve alone, especially if everyone around them insists “This is great news; you have to stick with it.” Depression might emerge as a way of signaling “I can’t handle this!” or of unwittingly sabotaging the untenable situation (the person’s performance collapses, forcing a reassessment). Childbirth is perhaps the most poignant example: it is a joyous event, yet postpartum depression is common, in part because a new baby imposes huge demands and some parents find they simply do not have the support or resources to meet those demands. The depressive reaction in this case can serve to alert the community that the new parents need help, or even, as one theory suggests, to subconsciously weigh the heartbreaking question of whether the parent can invest in this child at all under dire circumstances. In less tragic outcomes, a mother’s postpartum depression often lifts once additional support is provided – again consistent with the notion that the depression’s “goal” was to prompt a change in the social support system.
Across negative and positive triggers, a common theme is that the person’s social niche – their constellation of relationships, roles, and obligations – has become sub-responsive and is leaning into intransigence. Normal navigation and coping aren’t enough. Depression signals that a larger multi-party relational recalibration is needed. In mild cases, that recalibration might be achievable with some solitary soul-searching or a frank conversation. In severe cases, it may require a major renegotiation of multiple social contracts at once, which is no small feat.
Depression in the SNH framework is typically triggered by what we might call non–point-source entrapment—situations of chronic social or practical impasse that lack a single, solvable cause. Unlike an acute loss or one-off trauma, these are enduring predicaments (e.g. prolonged unemployment, oppressive social stigma, or untenable relationship conflicts) where the individual feels trapped with no clear escape. Such conditions often involve niche failure, signaling that one’s current social niche or life strategy is not viable. In these scenarios, depression functions as an evolved alarm: it flags the unlivable situation and halts “business as usual” behavior, forcing the individual to withdraw from futile efforts and reconsider alternative life strategies. This aligns with observations that feelings of defeat and entrapment strongly precipitate depressive episodes. In effect, SNH posits that depression is usually deployed when a person’s existing approach to life is untenable – a cue to change course rather than persist down a no-win path.
This emphasis on niche change also implies that depression should be selective, not a reflex to every kind of misery. In some of the harshest human environments, overt depression would be a bad bet. A person held in rigid, violently enforced slavery, for instance, confronts a “frozen” niche with almost no credible prospects for improvement and no partners who can be bargained with. To sink into non-functioning despair under such conditions would not move any gatekeeper and might invite further punishment. In those circumstances we would expect other defensive systems—fear, hyper-vigilance, submissive freezing, numb endurance—to carry the load, while the full social-bargaining aspect of depression is rarely engaged. By contrast, a person who is oppressed but retains some leverage and some allies—for example, a lower-status group member in a society that officially recognizes rights but often blocks their exercise—is in a much better position to use high-cost withdrawal as a bargaining chip. It is precisely in these ambiguous, partially negotiable entrapments that SNH predicts the most intense and recurrent depressive episodes. A similar logic applies to some gender-diverse adolescents in otherwise resource-rich families and communities: the socially recognized niche they need is visible and attainable in principle, but the local gatekeepers who control access resist or delay their transition; the result is a textbook case of non-point-source entrapment at the very life stage when long-term identity, partnership, and status are being forged.
The Challenge of Niche Change: Entrenched Partners and “Non-Point” Problems
Why does it often take something as drastic as depression to provoke niche change? One big reason is that humans are deeply averse to changing established social arrangements. Our lives are built on countless implicit contracts – who does what in the household, who earns money, who takes care of whom emotionally, what our status is among friends and colleagues, and so on. Even if these arrangements become inequitable or harmful, the people involved (including the suffering individual) often resist change because change is scary and disruptive. Most partners in a system prefer the predictability of the status quo. If you are the one suffering in a given arrangement, you might try ordinary negotiation – asking your spouse to treat you better, or asking your boss for a different assignment – but they might dismiss or deflect you, since any change could inconvenience them.
The Social Navigation Hypothesis pinpoints a particularly difficult scenario: when the constraints keeping you trapped are coming from multiple directions at once. It’s not just one villain you can confront or one simple fix. You might be, for example, a middle-aged adult with both work pressures and family pressures that conflict, or a person whose entire circle of friends engages in a lifestyle you find unsustainable, or an elder dependent on adult children who all subtly neglect you. In these cases, there is no single “point source” enemy to fight or flee; you are enmeshed in a web of constraints. This is precisely the kind of situation SNH sees as ripe for depression. When diffuse, multiple social partners all (perhaps unintentionally) reinforce a problematic niche, evolution’s answer was to hit the emergency brake – to become non-functional – thereby forcing all the partners to stop and reconsider their stance. The depression essentially forces a meeting (metaphorically speaking) among everyone involved, because ignoring it carries a cost for each of them.
It’s worth noting that depression is not always “successful” in achieving a better niche. Sometimes others do not come to the rescue or negotiate; they might abandon the person, replace them, or the depressed individual might remain chronically stuck if no resolution is possible. The SNH doesn’t claim that depression always yields a happy outcome – only that, on average in ancestral environments, this costly strategy paid off often enough to be selected for. In evolutionary terms, it was likely a strategy of last resort: used only when the situation was truly dire and every more conciliatory attempt had failed, which is why depression is relatively infrequent compared to normal sadness. And like any strategy, it can misfire. In the modern world especially, our social networks can be less cohesive and more anonymous. For example, a depressed worker may simply get fired rather than helped by an employer; a depressed individual might not have extended kin nearby to notice or intervene. These mismatches mean the adaptive “design” of depression may not always fit our current environment, leading to prolonged, unresolved depressions. This is an important caveat: saying depression has an evolutionary function does not mean it’s beneficial in every scenario. It only means it had a purpose, a fitness advantage, on average, under certain natural conditions, and understanding that purpose might help us address it more effectively now.
Why a ‘last resort’ strategy can still be common
At first glance, it might seem that a high‑gain, high‑cost program like major depression should be rare if it is an adaptation. Why would evolution give us such a risky tool and then let it fire as often as epidemiology suggests? The answer lies in how human social life is built.
Humans are not designed for socioeconomic stasis. Across the lifespan we acquire new skills, new knowledge, and new ambitions; we see possibilities our earlier selves could not have imagined. In principle, each such advance justifies a modest upgrade of our niche – more responsibility here, less drudgery there, a shift from one role to another. In practice, our socio‑economic niche is a dense matrix of exchange contracts with family, employers, partners, institutions. It is the bedrock on which our survival and reproductive plans rest. People therefore resist renegotiating it constantly, even when doing so would be fair and adaptive. Too much flux, and the bedrock turns into sand.
That combination – a mind that keeps learning and reaching, strapped to a contract network that quite rationally prefers stability – makes serious niche change both necessary and hard. Most of the time, we can muddle through with ordinary bargaining, friendly influence, and incremental adjustments. But not rarely, individuals find themselves in non–point‑source entrapments where a clearly better way of living is visible and yet blocked by a whole coalition of small vetoes. Those are not exotic edge cases; they are a predictable by‑product of being a long‑lived, innovative primate embedded in overlapping kin, economic, and moral systems.
From that vantage point, it would be more surprising if evolution had not built a powerful escalation tool. Major depression, in the SNH view, is that tool: a high‑gain mode reserved for those common but especially stubborn impasses where normal negotiation has failed. Its costs are large, but so are the stakes, and animal life is full of examples where organisms accept extreme risks when reproductive payoffs are high. The real puzzle is not why depression is common, but why so much of modern theory treats it as if such predicaments were rare. Maybe this occurs because thwarted niche change can superficially take on diverse appearances when, in fact, the same basic problem often is involved.
Misery is Not Enough
SNH implies a specific boundary condition: misery alone is not enough to trigger a major depression. Two key conditions have to be present to recruit the depressive adaptation: (1) the individual perceives a credibly better alternative to their current situation (a more promising social niche they could attain), and (2) there exist bargainable social partners who have the power to grant or block access to that better niche. If either condition—especially the second—is absent, the theory predicts the system will not deploy full-blown depression; instead, other responses to adversity will take the lead (such as fear and anxiety, rage, high-effort persistence, dissociation, or even submissive apathy). In plainer terms, if someone has absolutely no leverage and truly no one in their social world who can help them reach a better situation, becoming deeply depressed would be futile – and so evolution would favor other coping strategies in those cases. This perspective can shed light on certain epidemiological patterns: for instance, extremely oppressed or isolated populations might show lower rates of clinical depression than moderately oppressed ones (even if they are very unhappy), because if there’s truly “no way out,” the mind doesn’t bet on an expensive bargaining protest. Depression tends to emerge when there is something valuable and quite personal to fight for but is socially denied. Put another way: a slave in 18th-century Haiti had far less chance to improve their lot through bargaining than, say, a Black individual facing Jim Crow injustices in 1950s America who at least had some allies and legal avenues. SNH would predict more overt depression in the latter scenario, despite both being oppressive, because only in the latter were there credible partners and exits to bargain for.
A more extended treatment of this idea, with concrete group‑level examples (enslaved people, returning soldiers, working‑class whites, gender‑diverse youth), is given in the Critiques Essay: Box D: MDD Across Social Structures: An SNH‑Based Oppression Gradient.
Finally, even when depression does engage as designed, it may drag on if the social system around the person stubbornly refuses to change. Our modern institutions often “manage” or medicate away depressive signals without solving the underlying problem. The depressed person’s collapse might be absorbed by bureaucracy or viewed as purely a personal illness, rather than prompting a serious renegotiation of their life terms. In those cases, the person can remain stuck in depression much longer than would have happened in a tight-knit ancestral group. We will touch on these modern mismatches more in a moment.
Implications for Therapy and Support
Viewing depression through the lens of social navigation has practical implications for how we approach treatment and support for sufferers. First and foremost, it suggests that effective help must address the underlying social problems, not just the symptoms. If someone’s depression stems from being trapped in an unbearable role or from chronic neglect by loved ones, then therapy ideally should focus on identifying those stressors and finding ways to change the person’s niche to better suit them. This might involve working with the patient to set boundaries, communicate their needs more clearly to others, or even to exit toxic relationships or jobs. In fact, many existing depression therapies implicitly recognize this: for example, Interpersonal Therapy (IPT) for depression specifically looks at role transitions, disputes, and social role expectations – all within the realm of adjusting the patient’s social world. Likewise, good cognitive-behavioral therapists often help empower patients to assert themselves or to problem-solve practical life issues, not just challenge negative thoughts. From an SNH perspective, these approaches work because they align with the adaptive logic of depression: resolve the stalemate that triggered the depression, and the depression should abate. In essence, helping a patient “renegotiate their social contract” – whether that means dividing responsibilities more fairly with a spouse, seeking a different career path, or learning to ask friends for support – addresses the root causes that the depressive signal is screaming about.
Secondly, this perspective offers a more compassionate framing to patients and their families. Instead of viewing the depressed person as simply “sick” or “irrational,” we can ask: “What is this depression telling us about unmet needs or broken arrangements in this person’s life?” This doesn’t mean encouraging the person to remain depressed; it means listening to the signal. For example, if a teenager becomes depressed and withdraws, rather than only saying “Something’s wrong with your brain, let’s fix it,” parents might also consider what in the teen’s life is making them despair – are they being bullied at school (a conflict needing intervention)? Are they feeling unloved or under unbearable pressure (a sign the family dynamic needs adjustment)? The evolutionary view reminds us that feelings of despair are there for a reason, even if the reason is not immediately obvious. By hunting for that reason, we show respect for the sufferer’s experience and often discover real issues that can be improved. This approach can reduce blame and stigma: the patient isn’t “broken” or “weak” – rather, they are responding to something in their world that genuinely needs fixing.
What about medication? Antidepressant medications can be life‑saving tools—sometimes a person is so far down the well of depression that they need chemical help just to function enough to start making changes; in such cases relief is urgently necessary. The SNH perspective doesn’t oppose medication, any more than understanding that pain is adaptive would oppose using painkillers for someone with a broken leg. The new neurosteroid‑based treatments for postpartum depression illustrate this perfectly. In some cases, a short course of a GABA‑modulating drug can dissolve months of despair in a week or two by directly stabilizing hormone‑sensitive mood circuits. From an SNH point of view, that is a triumph at the proximate level: we are getting better at turning off an alarm that has become stuck on. But even here, the ultimate question remains: what were the pressures and support deficits that drove that system into crisis in the first place, and will they simply push it there again? If we only mute the symptoms without ever addressing the context that produced them, we risk leaving the person’s fundamental problem unsolved. In the alarm analogy, it is like silencing the siren without checking for the fire. Many clinicians have seen cases where medication lifted a patient’s mood just enough that they could tolerate an intolerable situation longer—but unless that situation changes, the depression often relapses or the person remains a shadow of themselves. Beyond even those grim endpoints, there is the quieter loss: we will never know what that person might have become had they been less heavily medicated at a potentially pivotal point in their life. Ideally, medication should be combined with efforts to change whatever was “burning” in that person’s life. Even the most ardent evolutionary theorists agree that nobody should suffer needlessly—if severe depression has spiraled into a self‑perpetuating biochemical hole, medication and other biological treatments are absolutely appropriate to stop the free‑fall. The key is what comes next: once the person can “breathe” again and can contribute more to their own development and problem‑solving, that reprieve should be used to fix the life problems that set off the alarm.
In practice, a therapy informed by SNH might involve very concrete social problem-solving. The therapist and patient might literally map out the person’s social world: Who are the allies? Who are the resistors? What conversations need to happen? Is there a way to get needs met that hasn’t been tried? Are there ways the person can signal their distress more clearly or, conversely, pull back in areas they’ve been overcommitted? Sometimes it might involve bringing in family members to educate them. For instance, telling a patient’s spouse: “Your partner’s depression is not just random – it may be responding to real issues between you. Let’s work on those, rather than you just expecting them to ‘snap out of it.’” In more severe or intractable cases, broader social interventions might be needed: for example, helping arrange childcare support for an overwhelmed mother, or connecting a lonely elder with community resources and social groups. The principle is that purely internal solutions won’t do if the causes are external and interpersonal. Smoothing the symptoms without changing the pressures is a band-aid at best.
Relationship to Alternative Theories
It is important to distinguish SNH’s account from other evolutionary explanations of depression. Mismatch theories hold that depression is largely maladaptive today because modern environments differ from the ancestral past; for example, contemporary social isolation or chronic work stress might trigger an ancient mood response that overshoots in intensity. SNH agrees that modern contexts (e.g. larger, looser social networks) can inflate depression’s frequency, but unlike mismatch models, it maintains that the core mechanism of depression remains a purposeful strategy rather than a broken alarm. Byproduct and genetic trade-off theories argue that depression itself wasn’t selected for, but is a side effect of other adaptations (such as high emotional sensitivity or the benefit of anxiety in small doses). For instance, Nettle’s review suggests depression persists because genes that increase neuroticism (and thus vigilance to risks) were favored, even though extreme neuroticism leads to depressive episodes. SNH, by contrast, posits direct adaptive functions for depressive symptoms, not merely side-effects – a claim that demands stronger evidence. Another viewpoint, the social rank theory, sees depression as an involuntary submission response: an adaptive yielding mechanism after defeat in status contests (to signal surrender and avoid further conflict). While rank theory overlaps with SNH (both acknowledge an evolved function in social contexts), SNH extends beyond status loss to any kind of entrenched social conflict of interest or deadlock. In SNH, depression is not just about accepting defeat; it’s about actively solving a stalemate – by recalibrating one’s goals and coercing reluctant partners if needed. Finally, traditional disease models treat depression as a pathology pure and simple – akin to diabetes or infection – with no adaptive value. This remains the prevailing medical view. SNH challenges it by noting that depression’s high prevalence and ancient lineage (across cultures and even other species’ analogues) suggest an evolved design, however costly, rather than a random glitch . These contrasts underscore that SNH is a bold claim on the adaptive side of the debate: it must show that depression has a coordinated functional logic that other models either misinterpret as dysfunction or only partially address.
Empirical Predictions of the SNH
Because SNH treats depression as an adaptation, it yields clear, testable predictions about when and how depressive episodes should occur. Key expectations include:
- Triggering Conditions: Depressive episodes should disproportionately follow entrapment-type stressors – enduring conflicts, humiliations, or blocked goals – rather than arbitrary traumas. Indeed, research finds that life events involving humiliation and feeling trapped are especially depressogenic , consistent with SNH. By contrast, if depression often struck without such insoluble triggers, or in trivial situations, it would challenge SNH’s adaptive logic.
- Problem-Solving Focus: Depressed individuals should exhibit intense rumination centered on their core problems. Some evidence supports this (depressed mood is linked to analytical, detailed thinking), but importantly, SNH predicts that this rumination can generate realistic solutions or insights. A failure to find any problem-solving benefit – for example, if depression uniformly produced only cognitive impairment with no analytic payoff – would count against the hypothesis.
- Social Assistance: If the social-signaling function is valid, we should see that support from others or concessions often precede recovery. Depression may elicit help or empathy from close associates (at least in ancestrally typical contexts). Accordingly, SNH would predict shorter or less severe episodes in environments where family/community support is readily given. Conversely, if studies showed that depressed behavior never elicits aid – or worse, always causes social rejection – it would undercut the idea of an evolved social benefit.
- Resolution and Recurrence: Once the underlying impasse is resolved, whether through the person’s own efforts or external help, SNH expects remission. From this perspective, the high rate of spontaneous remission in depressive episodes is not mysterious or embarrassing for functional accounts. It is exactly what one would expect if, in many cases, depression recruits intensive causal and strategic analysis and/or successfully triggers real movement in the social world (concessions, support, exits), either of which can make continued escalation unnecessary—a pattern supported by recent work that decomposes rumination into functional components.
- Non-Responsive Depression: If the constraining social matrix changes tangibly (documented concessions or exits) and yet the depression persists unabated, that suggests pathology rather than adaptive regulation. (We predict this will prove to be uncommon.) Likewise, SNH can be falsified if depression fails to terminate after its putative function is achieved. For example, if a depressive episode continues long after the individual has escaped the focal, fitness-limiting situation, it implies something has gone awry in the regulatory mechanism.
These criteria highlight failure conditions for SNH. In principle, finding large numbers of “unexplained” depressions – cases with no serious precipitating problem, no apparent analytical content, and no social or functional payoff – would indicate that depression is better explained as a dysfunction or byproduct. By spelling out what evidence would contradict it, SNH remains scientifically accountable. So far, the hypothesis is bolstered by observations that depression does often follow chronic stress and improves with problem-resolution, but definitive tests (for instance, whether depressed cognition actually yields better long-term decisions) remain an active research area.
Conclusion – Listening to the Signal
The Social Navigation Hypothesis reframes depression not as a mere defect, but as a desperate signal and catalyst for change when an individual’s life has hit an impasse. When someone’s social niche becomes unlivable – whether due to loss, mistreatment, impossible demands, or a collision of responsibilities – depression may emerge as an involuntary strategy of last resort. It forces a pause in ordinary life. It directs the sufferer’s mind inward to analyze the conflict. It broadcasts honest distress to anyone who might care. And if compassion alone doesn’t come, it withholds the person’s contributions, imposing costs on others until they are compelled to address the issue. In evolutionary terms, depression’s ultimate “goal” (so to speak) is to help the person navigate toward a more sustainable social niche – one in which their efforts and needs are in better balance. This mechanism can be triggered by a wide array of circumstances: being trapped in an unfair job or relationship, enduring a humiliating defeat, losing a key partner, or even facing the joyful burden of a new baby without sufficient help. In all cases, the depression is saying, “Something has to change, or I cannot go on.”
Recognizing this evolutionary logic does not mean glorifying depression or suggesting people should just endure it. On the contrary, it highlights how serious and real the sufferer’s problems are. A person in deep depression is not “lazy” or “weak” – their psyche is mounting a full-scale protest against a situation that is undermining them (or was perceived to be, at the precipice of the episode). When those around the depressed individual listen to that protest – when families, friends, or communities truly acknowledge the need, share the burden, and work to make changes – we often see depression ease dramatically. When the environment stubbornly refuses to change and only the symptoms are suppressed (for example, through medication alone), the person can remain stuck and the depression may persist or recur. In a way, the hypothesis urges us to treat a depressed person not just as a patient to sedate, but as a voice to heed.
Evolutionary thinking offers a compassionate and pragmatic lens: it suggests that we view depression sufferers as individuals whose pain has meaning – a meaning rooted in social needs and conflicts – rather than as broken machines. If we ask, “What is your depression telling us about your life?” we might get answers that lead to real solutions (like “I feel useless,” “I feel exploited,” “I feel alone”). We can then address those revelations directly, helping the person find purpose, assert their rights, or connect with others. In doing so, we aren’t indulging the depression; we are answering it. We are, in essence, negotiating with evolution’s alarm system – turning off the alarm not by cutting the wires, but by putting out the fire that triggered it.
Depression is, undeniably, ugly and painful. But seen through a focused and well-polished SNH lens, even its darkness may carry a hard-won wisdom. It tells us that human beings were not built to suffer silently in bad situations defeated by social complexity. We were built to signal need compellingly, to seek change, and to find a better way to live. By understanding and respecting that, we can better help those who suffer find hope and a healthier path forward.
In sum, the Social Navigation/Niche‑Change Hypothesis treats major depression, in its target domain, as a high‑gain social control system: it narrows attention to an entrapment problem, suppresses non‑instrumental rewards, and broadcasts escalating costs until partners renegotiate or the person exits. The clearest tests are correspondingly social: symptoms should track binding partner commitments and documented concessions/exits more closely than they track time, comfort, or generic rewards. When the environment moves, the mood system should move with it.
The Analytical Rumination Hypothesis (ARH) grew out of the original SNH. Appendix A provides a deep dive into the ARH and examines, after years of research on it as a stand-alone hypothesis, it now relates to the SNH as a whole.
Appendix A
Paul W. Andrews’ Analytical Rumination Program
and Its Relationship to the
Social Navigation / NicheChange Hypothesis
I am grateful that Paul W. Andrews was my first graduate student (co‑chaired with Randy Thornhill). Our work together, which even included a Flathead Lake Biostation summer of field and CO₂‑respirometry‑based lab work on Sierra dome spider copulatory‑courtship energetics and discretely variable bumblebee respiratory patterns, culminated in Watson & Andrews (2002). That paper, the product of several years’ work, put before the psychiatric community what later came to be called the Social Navigation / Niche‑Change Hypothesis (SNH) of depression. In its original three‑fold framing, what we now label (a) depressive “analytical rumination,” (b) bargaining / honest signaling, and (c) extortion / sanction were never meant as separate theories. They were always intended as tightly coupled facets of a single adaptation.
Over the following decades Paul’s career came to focus on the cognitive component of that package. In Andrews & Thomson (2009) this strand crystallized as the Analytical Rumination Hypothesis (ARH): a relatively self‑contained account of depression as an evolved mode of problem solving. This appendix briefly reviews what that empirical program has actually shown, where I think it falls short when treated in isolation, and how it fits into the broader SNH architecture as I now see it. – PJW
1. ARH in brief
ARH starts from a simple but important observation: depressive episodes are not randomly triggered. They are disproportionately associated with serious, complex problems—often social or personal dilemmas—with large potential consequences and no obvious solution. Once such an episode is triggered, ARH proposes that three things happen.
1.Withdrawal from business‑as‑usual. Everyday pursuits lose some of their pull, and attention turns inward.
2.Narrowing of focus. Attention is pulled toward the precipitating problem and its surrounding circumstances.
3.Recruitment of a particular style of thinking. This style is both causal (“Why did this happen?” “What did I do?” “What bigger pattern am I in?”) and strategic (“What can I change so this does not happen again?” “What are my options?”).
On this view, depressive rumination is not mere repetitive self‑torment. It is a distraction‑resistant analytic mode designed to stay locked onto the hardest current problem until the sufferer has understood it well enough to identify a viable response. Symptoms such as anhedonia and psychomotor slowing are reinterpreted as part of the cost of this deep focus, not as pure malfunction.
That picture yields two straightforward empirical expectations:
•Trigger structure. Depressed people should be facing more complex, entangled problems than non‑depressed people, and should report more causal analysis of those problems.
•Functional payoff. Those who do more structured, solution‑oriented thinking about their precipitating problems should ultimately fare better, at least in terms of symptom relief.
2. What Andrews’ et al. empirical work has actually shown
2.1 Measurement: separating “brooding” from problem‑solving
A key early move in Andrew’s program was to argue that standard rumination scales do not carve the phenomenon along the lines ARH cares about. The widely used Ruminative Responses Scale (RRS), with its “brooding” and “pondering” factors, mixes different kinds of causal‑analysis items and never really isolates a genuine problem‑solving dimension. If you then correlate that undifferentiated lump with outcomes, it is easy to conclude that “rumination is toxic.”
Bartošková, Andrews and colleagues (2018) make this “bad instrument → bad inference” point unusually explicit. They show that to test ARH properly you need a scale that actually contains separable causal-analysis and problem-solving-analysis components; Andrew’s and colleagues presented a proper scale in 2014. They compare the widely used Ruminative Responses Scale (RRS) to the newer Analytical Rumination Questionnaire (ARQ) across five samples drawn from two cultures (Canada, Czech Republic) and mixed clinical status (nonclinical and hospitalized; total N ≈ 1414). The ARQ shows the expected two-factor structure (causal analysis and problem-solving analysis), making it suitable for testing ARH’s predicted covariance pattern. By contrast, the RRS factors do not reliably behave like “problem-solving,” and when the authors try to reproduce the ARH-predicted cyclical pattern using RRS brooding/pondering, the key feedback relation is systematically weak, absent, or even reversed. The central methodological punchline is that one cannot adjudicate “rumination is maladaptive” until one has measured the right kind of rumination.
Using Rasch analysis and factor analysis on five samples from Canada and the Czech Republic (student, online, and hospitalized), Andrews and colleagues validated a theory‑driven instrument, the Analytical Rumination Questionnaire (ARQ). Across those samples, rumination reliably split into two latent factors:
•Causal analysis – effortful thinking about why the problem arose, what deeper pattern is at work, what one did wrong.
•Problem‑solving analysis – thinking through constraints, options, and how to prevent similar outcomes in future.
Both factors emerged cleanly across cultures and clinical status, and both were positively associated with depressive symptoms. The more depressed people were, the more they engaged in exactly the kind of root‑cause analysis and constrained problem‑solving that ARH and SNH had always proposed are central to the syndrome.
When they tried to run the same structural models with the RRS brooding/pondering factors, the functional pattern largely disappeared. On ARQ, depressive symptoms were positively related to causal analysis, which in turn was positively related to problem‑solving analysis, and—critically—problem‑solving analysis showed a negative association with depression when everything was modeled together. In rough path terms:
depression → causal analysis → solution analysis → reduced depression.
On RRS, those relationships were muddied. This is one of the places where I think Andrews is clearly right: bad constructs can make functional relationships look maladaptive.
There is also a subtler statistical point in Bartošková et al. (2018) that is worth surfacing, because it explains why even well-meaning analysts can miss the functional signal. When you look only at the bivariate association between depression and problem-solving analysis, the correlation is often weak or non-significant. These investigators argue this can happen because there are two opposing sources of covariance operating at once: a positive association mediated by causal analysis (more depression → more causal analysis → more problem-solving analysis), and a negative “direct” association between depression and problem-solving that runs in the opposite direction. Those can partially cancel, producing the misleading surface impression that depression is unrelated to problem-solving or slightly suppresses it. Their broader point is that you don’t learn much about function by eyeballing simple correlations when the system has coupled sub-components with opposite-signed effects; you have to model the structure.
2.2 Clinical samples: complex problems and “busy minds”
In a 2020 longitudinal study of hospitalized patients with major depression, Andrews’ group asked whether this analytical style merely co‑occurs with depression or actually feeds into recovery.
Key points:
•Problem load and complexity. Severely depressed inpatients reported more numerous and more complex problems than matched non‑depressed controls. Their difficulties were multi‑factor, multi‑partner, and chronic rather than one‑off hassles. That is exactly what any adaptive model would expect: the system is being recruited in the presence of unusually thorny, high‑stakes situations.
•Analytic engagement. These patients reported substantially more causal analysis—more “Why did this happen?” thinking—about their difficulties than controls. That part of the ARH picture is clearly supported: depression is not simply a fog; it is associated with intensive, cause‑focused thinking about the precipitating problems.
•Problem‑solving analysis. Perhaps more surprisingly, inpatients did not report less solution‑oriented thinking than non‑depressed controls. On measures of goal‑directed problem‑solving analysis—deliberation about what to do, how to change things, how to avoid similar outcomes—depressed patients were at least as strategically engaged as those without depression. That alone already undermines the crude stereotype of major depression as a state of pure cognitive paralysis. If anything, severely depressed people appear to have busy minds, not empty ones.
On the more demanding question—does any of this rumination actually help?—the picture is mixed but not null:
•Within the inpatient sample, higher levels of problem‑solving analysis at intake predicted greater improvement in mood by week five of treatment, even after controlling for initial severity and problem complexity. In other words, among people who were already depressed, those doing more solution‑focused thinking tended, on average, to get somewhat better faster.
•At the same time, the objective complexity of people’s problems did not collapse in lockstep with rumination, and patients dealing with the most entangled, multi‑party dilemmas often remained depressed despite high levels of analysis.
•Some of the apparent benefits weaken under more conservative statistics. The safest summary is: there is clear evidence that depressed people engage in focused causal and solution‑oriented thinking, and some evidence that this can predict modest symptom relief, but no strong evidence yet that depressive rumination reliably “solves” people’s life problems or yields better real‑world outcomes than would have occurred without the episode.
2.3 Experimental “mini‑syndromes” and cognitive trade‑offs
More recent experimental work from Paul and others has tried to induce short‑lived “mini‑syndromes” in the lab using social rejection or betrayal paradigms. In these designs, participants experience a controlled interpersonal slight (for example, being excluded from a ball‑tossing game or exposed to a betrayal narrative), and mood, rumination, and task performance are followed over hours or days.
The recurring pattern is:
•modest but reliable increases in sadness and loss of positive affect,
•increased use of negative‑emotion and self‑blame language when writing about the event,
•more causal reconstruction (“what went wrong, why”) in those narratives, and
•small decrements in performance on unrelated cognitive tasks, consistent with some capacity being tied up by self‑generated analysis of the social slight.
From an SNH standpoint, this is an interesting but narrow proof of concept. These paradigms capture the very early edge of an episode: detection of a social problem (“they excluded me”), subjective sense that something is wrong, and a surge of root‑cause analysis, with measurable cost to other cognition. They do not model:
•non‑point‑source, multi‑partner entrapment,
•weeks‑to‑months‑long bargaining campaigns,
•the deeper sensory flattening and motor changes of advanced anhedonia, or
•real negotiations and actual niche change.
In short, they show that mild, induced dysphoria organizes thought around social slights and draws energy away from other tasks—consistent with ARH—but they leave the SNH “heavy machinery” largely unexpressed.
2.4 Rumination and generic cognitive performance
A related theme in Andrews’ writing is how to interpret depressed patients’ poor performance on standard lab tasks of memory, attention, and executive function. The usual inference is: “depression impairs cognition.” ARH suggests a different reading:
•A great deal of scarce cognitive resource is being spent on self‑generated analysis of real problems.
•“Spare” capacity for experimenter‑chosen tasks is therefore reduced.
•When opportunities to ruminate are constrained, or when tasks are tightly tied to the person’s live social dilemma, some of the apparent deficits shrink.
That pattern is more consistent with a reallocation of effort than with a global collapse of analytic capacity. Again, this does not show that depression makes people better problem‑solvers than everyone else; it shows that, even when very ill, they are not cognitively inert.
On the social‑perception side, complementary work by Hagen and colleagues has examined how third parties read depressive behavior. In factorial vignette studies, observers read about interpersonal disputes where the victim either did or did not respond with depressive collapse or self‑harm threats. Across cultures and samples, presence of depressive or self‑harming behavior reliably increased:
•perceived genuineness of suffering,
•judgments that the victim was less manipulative and more deserving of help, and
•willingness to offer support or make concessions.
That is exactly what a credible‑signal model would predict. From an SNH perspective, these findings are not the whole story—we still need longitudinal data on actual concessions, exits, and niche change—but they are a proof of concept that depressive behavior functions, in observers’ minds, as a trustworthy signal of need, not as meaningless noise.
3. Recurrence, homeostasis, and antidepressants
A second strand of Andrews’ work, especially in the “Blue Again” meta‑analysis, tackles recurrence and drug effects.
The key concept is oppositional tolerance. If depression is regulated by a functioning homeostatic system rather than a broken one, then drugs that forcibly shift monoamine levels should elicit compensatory reactions that push back toward the prior equilibrium. When the drug is withdrawn, those compensations can overshoot, producing a rebound into depression that is more likely or more intense than an unmedicated baseline.
The meta‑analysis finds exactly this pattern:
•People who achieve remission on antidepressants and then discontinue them have substantially higher relapse rates than those who remit without medication.
•Drugs that produce larger perturbations of monoamine systems are associated with higher post‑discontinuation relapse.
From an adaptation‑aware perspective, that looks less like a broken system being fixed and more like a functioning control system pushing against an artificial perturbation. Andrews is careful not to claim that this proves depression is adaptive, but he does reasonably conclude that these relapse dynamics provide no positive evidence of malfunction in the monoamine‑regulation machinery.
Two points follow for SNH (and for any evolutionary account):
•The mere fact of recurrence, especially after discontinuation of a drug that has forcibly altered brain chemistry, cannot be lazily cited as proof the underlying system is defective. Some portion of that recurrence is almost certainly produced by normal homeostatic feedback.
•A functioning social‑navigation system ought to be reusable. Humans can encounter multiple episodes of non‑point‑source entrapment over a lifetime and can re‑enter similar structures after partial escapes. From an SNH perspective, repeated episodes are often repeated campaigns—renewed attempts to renegotiate or exit fresh or still‑unresolved traps—rather than simple evidence that the mechanism is diseased.
None of this denies that some depressive states are genuinely malignant, self‑perpetuating, and very likely misfires. The question is how often that is the case. Andrews’ meta‑analytic work makes it harder to treat recurrence by itself as decisive evidence against adaptation.
4. Where ARH, taken alone, still falls short
Critics of adaptive theories often assert that there is “no empirical evidence” that depression helps people solve problems. ARH decisively undermines that sweeping claim. We now have solid evidence that:
•depressed individuals face more complex problems,
•their thought is systematically oriented toward those problems in causal and strategic terms, and
•in at least some samples, greater problem‑solving analysis predicts better symptom trajectories.
However, if ARH is presented as the adaptive story—“depression exists to make you a better problem‑solver”—it still shoulders an evidentiary burden it has not yet met.
Specifically:
•We do not yet have good evidence that depressive rumination reliably yields better real‑world outcomes: more effective resolution of the triggering social dilemma, better long‑term decisions, or measurable gains in proxies for inclusive fitness.
•The mainstream clinical literature continues to find that most forms of depressive rumination predict worse trajectories: more persistent symptoms, more anxiety, greater risk of suicidality ((Nolen-Hoeksema, 1991; Nolen-Hoeksema et al., 2008; Watkins, 2008). Andrews has argued, with substantial empirical support, that many of these measures confound problem-solving analysis with generic self-focused brooding. Even so, the key question remains: a functional claim ultimately has to show net benefit, not just structured thought.
In my view, this gap between a sharp functional story and mixed outcome data is the main reason much of the field remains skeptical of ARH when it is treated as the primary adaptive account of depression.
5. How SNH uses and modifies Andrews’ ideas
The Social Navigation / Niche‑Change Hypothesis takes Andrews’ strongest insights and embeds them in a different architecture.
In the original Watson & Andrews (2002) formulation, what later became “analytical rumination” was always Phase 1 of a three‑part system:
1.a distraction‑resistant, problem‑focused cognitive mode;
2.an honest signal of need and commitment expressed through visible distress and withdrawal; and
3.if those honest signals fail, an involuntary sanction that withdraws contributions and imposes costs on unresponsive partners until they concede or make exit feasible.
In real life these “phases” are not rigid steps but braided functions. From the first days of an episode:
•analytical rumination,
•honest signaling, and
•sanction‑like withdrawal
can all be present to varying degrees in different parts of the person’s social world. One partner mainly encounters Phase 1—long, searching conversations about what has gone wrong. Another mainly sees Phase 2—visible distress and credible pleas for help. A third mainly feels Phase 3—missed obligations, loss of warmth, or outright non‑cooperation.
In that three‑function design, rumination is vital but not expected to carry the whole adaptive load by itself. Its jobs are to:
•strip away rosy illusions about the current niche,
•clarify which alternative arrangements would be better and what concessions or exits would be required from whom, and
•prepare the sufferer to evaluate proposals when they arrive.
From an SNH point of view, it is not surprising that many depressed people do not, on their own, “solve” their most complex social dilemmas. The problems that trigger major depression under this model—non‑point‑source entrapments involving multiple interlocking partners and institutions—are precisely those that no single mind can readily resolve solo. They require cooperation.
SNH therefore shifts the success criterion. The key question is no longer:
“Does rumination make the individual a better solitary problem‑solver?”
but rather:
“Does the full depressive episode, including its signaling and sanctioning phases, increase the odds that the person’s social world actually changes in ways that move them toward a better niche?”
Progress is measured in concessions, support, and exits, not just in private insight
This reframing also changes what counts as a critical test. ARH tends to be evaluated with lab tasks and short‑term symptom scores. SNH points us instead toward studies that:
•track whether depressive episodes arising from complex non‑point‑source entrapments are followed by documented changes in workload, authority, resource access, living arrangements, or partner behavior; and
•ask whether symptom relief tracks those concrete changes—the Concession/Exit patterns—more closely than it tracks generic encouragement, medication, clever verbal manipulation, or time.
Those are demanding studies, but conceptually clearer. They test whether depression, in its intended domain, actually does social‑navigation work.
6. Abstract vs. concrete rumination
Analytical rumination needs one more refinement that newer literature makes hard to ignore. Work on “levels of construal” shows that not all rumination is the same (Watkins, 2008):
•Abstract rumination (“Why am I like this?” “Why do people always treat me this way?”) is vague, global, and self‑evaluative.
•Concrete rumination (“What exactly happened at that meeting?” “Who said what?” “What can I try next time?”) is specific, situational, and action‑linked.
Across studies:
•abstract rumination is reliably associated with higher depressive symptoms and more indecisiveness (Watkins, 2008; Winchell and Ezawa, 2025),
•concrete rumination is either weakly related to symptoms or modestly protective, especially in highly indecisive people (Winchell and Ezawa, 2025).
Experimental inductions tell a similar story: when depressed participants are nudged into a concrete processing mode, they generate more solutions and more effective plans for social problems than when they are held in an abstract “why” mode (Watkins, 2008).
Taken together, this pushes us to read “analytical rumination” in the ARH/SNH sense as primarily concrete causal–strategic thinking, not endless global self‑critique (Watkins, 2008).
That does not mean abstract rumination has no role. One might say that a “vision quest” whose goal is to discover one’s place in the community, if not the entire cosmos, is a socially sanctioned form of abstract rumination (and maybe a tradition that mitigates against mild or incipient major depression). In real episodes people probably move back and forth: some degree of higher‑level “what does this mean about my life?” thinking may be necessary to notice that one’s niche is untenable at all.
Abstract rumination is not necessarily a derailment of the depressive process; in major niche-change scenarios it may be an essential preparatory phase.
In those major niche-change scenarios, abstract, existentially flavored rumination may serve a preparatory function: helping the individual detach from identities, relationships, and sources of meaning embedded in the current niche. Before concrete planning can proceed, the person may need to confront what will be lost, not just what might be gained. From an ARH/SNH perspective, depression’s capacity to flatten pleasure and loosen emotional attachments, and to concentrate the mind on serious existential questions, may be part of what enables a person to contemplate leaving behind a life that is familiar, valued, and even loved, but no longer viable from an inclusive-fitness standpoint—often only dimly represented in conscious awareness. In this sense, abstract rumination may prepare the organism for inner transformations, and for the emotionally difficult realities of renegotiation, exit, and—sometimes—relationship loss, not merely for the still necessary follow-on strategically navigational and tactical problem-solving. It is conceivable that the more abstract forms of rumination even may be responsible for some early remissions.
The trouble comes when the system gets stuck too long—when time is passing, opportunity costs are mounting, and performance in the current niche is deteriorating—so abstract rumination combines with aversive indecisiveness and no descent into concrete planning occurs. (In other words, whether rumination helps or harms depends on whether it is coupled to decisive movement toward concrete action; when indecision persists, abstract rumination amplifies symptoms rather than facilitating resolution; Winchell & Ezawa, 2025.). On the SNH picture, that is precisely where wise others are supposed to matter: a good therapist, elder, or ally helps work through existential concerns, translate diffuse, self‑blaming loops into specific, testable hypotheses and next steps (“Let’s list the actual contracts that are failing; who could we recruit?”).
We do not yet have good naturalistic data on how often abstract rumination, unaided, evolves into concrete problem‑solving in everyday life; that transition is largely a theoretical postulate and an important empirical gap. But the construal‑level findings sharpen the prediction: when depressive episodes show a shift toward detailed, situation‑specific analysis and experiments in niche change, ARH/SNH should fare better; when people are marooned in global “why” thinking, the adaptive logic has stalled and help is needed to restart it (Watkins, 2008; Winchell and Ezawa, 2025).
7. Why splitting off “analytical rumination” cripples the test
A further problem with treating the Analytical Rumination Hypothesis as a stand‑alone theory is that it implicitly amputates the regulatory machinery that, in SNH, controls the whole depressive triad.
The adaptation we are talking about is not a free‑floating “rumination module.” It is a coordinated package:
•focused social‑causal analysis,
•honest signaling of need,
•non‑volitional sanctions, and
•the control systems that decide when to recruit each element, how much they should overlap, how hard to drive them, and when to stand the system down in response to how the social world actually behaves.
Those regulatory mechanisms are not tidy boxes; they are intertwined. In a real episode the brain is constantly adjusting phase overlap and gain. For example:
•If early signaling brings genuine help, sanctions may never fully engage.
•If the network stonewalls, sanctions intensify while conscious rumination may partially shut down.
•If partners move but only halfway, the system may hold a lower‑level depressive state while testing whether the new contracts are stable.
That fine‑tuning is where a lot of the “effectiveness, efficiency, and design specificity” that Williams talked about actually lives.
Standard lab paradigms do not allow that regulatory system to operate. Short film inductions, Cyberball rejection, or artificial problem‑solving tasks are typically:
•low‑stakes and reversible,
•based on interactions with strangers or outright fictional partners,
•divorced from real contracts or long‑term roles, and
•confined to an hour or two, with no genuine possibility of niche change.
In that setting, the adaptation never fully turns on. There is no real social network for the signal‑and‑sanctions phases to act on, no convenors with power, and no time horizon over which regulatory adjustments could express themselves. What gets measured is at best a weak, context‑free trace of rumination, stripped of its normal inputs and outputs.
It is therefore not surprising that under those constraints we often fail to see clear improvements in problem‑solving or neat mappings from trigger to outcome. We are effectively testing a heart valve on a table and concluding from its poor job of supporting locomotion that “hearts are not well designed for running.”
For SNH, this means that lab tests which isolate “rumination” from the larger social‑navigation system are systematically biased against detecting the adaptation’s true design. The appropriate tests are those that let the full package operate: episodes unfolding over weeks or months in real communities, with real contracts at stake, where the regulatory mechanisms can decide how much to overlap the three phases and adjust their gain in response to actual partner behavior.
Only in that kind of setting can we fairly ask whether the depression system shows the effectiveness, efficiency, and specificity that mark it as a product of selection.
8. Recurrence through the joint lens of ARH and SNH
Seen through the combined ARH/SNH lens, recurrence looks less mysterious.
•ARH reminds us that depression is regulated by a homeostatic neurochemical system that pushes back against drugs in ways that look like a functioning controller, not a smashed one.
•SNH reminds us that the ecology of deployment is messy: people can fall into multiple traps across a life, can re‑enter traps they once escaped, and can have their bargaining campaigns truncated by interventions that change mood but not niche.
From this joint standpoint:
•Some recurrences are almost certainly iatrogenic—products of oppositional tolerance after medication is withdrawn, with no implication that the system was intrinsically broken.
•Some recurrences are just what you would expect of a reusable bargaining tool in a social world that keeps producing exploitive, blocked, or collapsing roles.
•Some episodes—especially the very chronic, triggerless ones—probably are misfires or mismatches: cases where the switch gets stuck or the modern environment provides no way for the strategy to succeed.
The empirical task is to sort these pathways, not to assume that recurrence, in and of itself, can tell the whole story.
9. Where things stand now
So where does this leave Andrews’ analytical rumination program relative to SNH?
1.On the credit side:
•His work has decisively undermined the easy claim that “there is no evidence whatsoever that depression aids problem solving.”
•We now have solid evidence that depressed individuals are not cognitively inert; their thought is systematically oriented toward complex, real problems; and in at least some contexts, greater problem‑solving analysis predicts better symptom trajectories.
•We also have serious grounds, via the oppositional‑tolerance work, to doubt the picture of depression as a simple monoamine defect. The regulation looks like a functioning control system, even if we do not yet fully understand what it is trying to achieve.
2.On the limitation side:
•ARH, if treated as the adaptive story, still over‑promises. It has not yet shown that the costs of major depression are reliably offset by cognitive gains that manifest in better real‑world outcomes.
•As long as the theory is framed as “depression exists to make you a better problem solver,” skeptics will have an easy time pointing to the many cases where depressed thinking looks stuck, circular, or distorted.
3.On the integration side:
•SNH is, in my view, where Andrews’ strongest insights naturally belong: as Phase 1 of a larger, explicitly social adaptation. In that context, the fact that depressed minds are deeply engaged with their problems is not expected to carry the whole adaptive weight. It is part of a sequenced strategy that includes honest signaling of need and, where necessary, extortionary withdrawal of benefits until partners move.
•Evaluated on that broader criterion—“Does depression, in the right kind of situation, help restructure a failing niche?”—the theory becomes both more plausible and more empirically tractable.
One nice implication the 2018 paper draws is that the high rate of spontaneous remission is not automatically embarrassing for analytical models. If depression tends to recruit a two-stage sequence—first causal analysis, then constrained solution-generation—then many episodes should decline once enough causal structure is discovered and at least some viable solution path is selected, even without formal intervention. That is not a claim that depression is “good,” only that the observed tendency for episodes to end is consistent with a system that is doing work and then standing down when the work is “good enough.
Finally, the empirical agenda that follows from combining ARH with SNH is clear. We now need studies that look not just at what depressed people think, but at what others do in response, and at whether symptom relief tracks documented concessions and exits that mark real niche change. Only then will we be able to say how often this ugly, costly response achieves what, in SNH terms, it was built to do.
Select References for
Positive Case and Critique Essays
Core Social Navigation / Bargaining / SNH Materials
Hagen, E. H. (1999). The functions of postpartum depression. Evolution and Human Behavior, 20(5), 325–359.
Watson, P. J., & Andrews, P. W. (2002). Toward a revised evolutionary adaptationist analysis of depression: The social navigation hypothesis. Journal of Affective Disorders, 72(1), 1–14.
ClineBrown, K., & Watson, P. J. (2005). Investigating major depressive disorder from an evolutionary adaptationist perspective: Fitness hindrances and the Social Navigation Hypothesis. In J. T. Devito (Ed.), Focus on depression research (pp. 15–44). New York, NY: Nova Biomedical Books.
Hagen, E. H. (2003). The bargaining model of depression. In P. Hammerstein (Ed.), Genetic and cultural evolution of cooperation (pp. 95–123). Cambridge, MA: MIT Press.
Hagen, E. H. (2011). Evolutionary theories of depression: A critical review. Canadian Journal of Psychiatry, 56(12), 716–726.
Hagen, E. H., Watson, P. J., & Thomson, J. A. (2004). Love’s labour’s lost: Depression as an evolutionary adaptation to obtain help from those with whom one is in conflict. (Unpublished manuscript, latest version 20 May 2004).
Watson, P. J., Andrews, P. W., Hagen, E. H., & Thomson, J. A. (ca. 2004). Depression as an evolutionary strategy. (Manuscript submitted to The Lancet; unpublished).
Watson, P. J., Andrews, P. W., Hagen, E. H., & Thomson, J. A. (ca. 2004). Depression and social navigation: An evolutionary hypothesis. (Manuscript submitted to Archives of General Psychiatry; unpublished).
Analytical Rumination & Andrew’s Program
Andrews, P. W., & Thomson, J. A., Jr. (2009). The bright side of being blue: Depression as an adaptation for analyzing complex problems. Psychological Review, 116(3), 620–654.
Andrews, P. W., & Thomson, J. A., Jr. (2010). Depression’s evolutionary roots. Scientific American Mind, 20(4), 56–61.
Andrews, P. W., Kornstein, S. G., Halberstadt, L. J., Gardner, C. O., & Neale, M. C. (2011). Blue again: Perturbational effects of antidepressants suggest monoaminergic homeostasis in major depression. Frontiers in Psychology, 2, 159.
Barbic, S. P., Durisko, Z., & Andrews, P. W. (2014). Measuring the bright side of being blue: A new tool for assessing analytical rumination in depression. PLOS ONE, 9(11), e112077.
Bartosková, M., Ševčíková, M., Durisko, Z., Maslej, M.M., Barbic, S.P., Preiss, M., & Andrews, P. W. (2018). The form and function of depressive rumination. Evolution and Human Behavior, 39(3), 277–289.
Andrews, P. W., Maslej, M. M., Thomson, J. A., Jr., & Hollon, S. D. (2020). Disordered doctors or rational rats? Testing adaptationist and disorder hypotheses for melancholic depression and their relevance for clinical psychology. Clinical Psychology Review, Volume 82, 101927.
Hollon, S. D., Andrews, P. W., Singla, D. R., et al. (2021). Evolutionary theory and the treatment of depression: It is all about the squids and the sea bass. Behaviour Research and Therapy, 143, 103849.
Sevčíková, M., Loučka, M., Durdisová, M., & Andrews, P. W. (2020). Testing the analytical rumination hypothesis: Exploring the longitudinal effects of problemsolving analysis on depression. Frontiers in Psychology, 11, 1344.
Altman, M., Martin, L., Chiu, C., Northover, S. B., Huang, S., Goegan, S., Maslej, M. M., Hollon, S. D., Mulsant, B. H., & Andrews, P. W. (2024). An experimental paradigm for triggering a depressive syndrome. Emotion. Advance online publication.
Nolen-Hoeksema, S. (1991). Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology, 100(4), 569–582.
Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3(5), 400–424.
Watkins, E. (2008). Constructive and unconstructive repetitive thought. Psychological Bulletin, 134(2), 163–206.
Signaling / Suicidality / Selfharm
Hagen, E. H., Watson, P. J., & Hammerstein, P. (2008). Gestures of despair and hope: A view on deliberate selfharm from economics and evolutionary biology. Biological Theory, 3(2), 123–138.
Gaffney, M. R., Adams, K. H., Syme, K. L., & Hagen, E. H. (2022). Depression and suicidality as evolved credible signals of need in social conflicts. Evolution and Human Behavior, 43(3), 242–256.
Soper, C.A., Shackelford, T.K. (2023). Are depression and suicidality evolved signals? Evidently, no. Evolution and Human Behavior, 44(2), 147-154,
Gaffney, M. R., Adams, K. H., Syme, K. L., & Hagen, E. H. (2023). Response to: “Are depression and suicidality evolved signals? Evidently, no.” Evolution and Human Behavior, 44(2), 155–160.
Broader Evolutionary Psychiatry / Levels of Analysis
Price, J. S. (1967). The dominance hierarchy and the evolution of mental illness. The Lancet, 290(7506), 243–246.
Sherman, P. W. (1988). The levels of analysis. Animal Behaviour, 36(2), 616–619.
Varga, S. (2012). Naturalism, interpretation, and mental disorder: Philosophical essays on the DSM. New York, NY: Oxford University Press.
Price, J. S., & Sloman, L. (1987). Depression as yielding behavior: An animal model based on SchjelderupEbbe’s pecking order. Ethology and Sociobiology, 8(Suppl.), 85S–98S.
Brown, G. W. (2002). Social roles, context and evolution in the origins of depression. Journal of Health and Social Behavior, 43(3), 255–276.
Brown, G. W., Harris, T. O., & Hepworth, C. (1995). Loss, humiliation and entrapment among women developing depression: A patient and nonpatient comparison. Psychological Medicine, 25(1), 7–21.
Keller, M. C., & Nesse, R. M. (2006). The evolutionary significance of depressive symptoms: Different adverse situations lead to different depressive symptom patterns. Journal of Personality and Social Psychology, 91(2), 316–330.
Allen, N. B., & Badcock, P. B. T. (2003). The social risk hypothesis of depressed mood: Evolutionary, psychosocial, and neurobiological perspectives. Psychological Bulletin, 129(6), 887–913.
Allen, N. B., & Badcock, P. B. T. (2006). Darwinian models of depression: A review of evolutionary accounts of mood and mood disorders. Progress in NeuroPsychopharmacology & Biological Psychiatry, 30(5), 815–826.
Rosenström, T. (2013). Bargaining models of depression. Journal of Theoretical Biology, 331, 54–65.
Kennair, L. E. O., Kleppestø, T. H., Larsen, S. M., et al. (2017). Depression: Is rumination really adaptive? In T. K. Shackelford & V. ZeiglerHill (Eds.), The evolution of psychopathology (pp. 73–92). Berlin: Springer.
Critiques of Adaptive Accounts & MetaDebates
Nettle, D. (2004). Evolutionary origins of depression: A review and reformulation. Journal of Affective Disorders, 81(2), 91–102.
Nettle, D. (2004) Adaptive illusions: optimism, control, and human rationality. In D. Evans & P. Cruse (Eds.), Emotion, Evolution, and Rationality (pp. 193-208) Oxford Univ. Press
Hagen, E. H., & Thomson, J. A., Jr. (2004). Social navigation hypothesis of depression revisited. Journal of Affective Disorders, 83(2–3), 285–286.
Nettle, D. (2009). An evolutionary model of low mood states. Journal of Theoretical Biology, 257(1), 100–103.
Kleppestø, T.H. (2014). Why does depression exist? A review with new predictions from evolutionary theories. Master Thesis. The University of Bergen.
Haselton, M. G., & Nettle, D. (2015). The paranoid optimist: An integrative evolutionary model of cognitive biases. In D. M. Buss (Ed.), The handbook of evolutionary psychology (2nd ed., Vol. 1, pp. 123–142). Wiley.
Nesse, R. M. (2023). Evolutionary psychiatry: Foundations, progress and challenges. World Psychiatry, 22(2), 177–202.
Winchell, B., & Ezawa, I. D. (2025). Indecisiveness moderates the relationship between rumination modes and depressive symptoms. Frontiers in Psychology, 16, 1681121.